Abstract
CT-guided tumor ablation is one of the most challenging developments in the field of interventional radiology. The radiologist performing tumor ablation needs profound knowledge both in modern diagnostic and interventional radiology and in clinical and oncological patients care. These premises have to be fulfilled to be an accepted partner especially for the surgeons—who often think that they are in competition for patients qualifying for minimally invasive therapies with interventional radiologists—as well as for the referring oncologists.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
CT-guided tumor ablation is one of the most challenging developments in the field of interventional radiology. The radiologist performing tumor ablation needs profound knowledge both in modern diagnostic and interventional radiology and in clinical and oncological patients care. These premises have to be fulfilled to be an accepted partner especially for the surgeons—who often think that they are in competition for patients qualifying for minimally invasive therapies with interventional radiologists—as well as for the referring oncologists.
Ablation is the deposition of energy into a tumor using percutaneous electrodes, antennae, or probes with the intent of destroying the tumor and a margin of normal surrounding tissue. Thermal ablative techniques using heat (laser, radiofrequency, microwave) or cold (kryotherapy) showed a rapid progress during the last 20 years with its efficacy being confirmed by multiple large series and clinical follow-up since then. Especially in patients suffering from HCC in underlying liver cirrhosis there was early proof that radiofrequency ablation is superior to open surgery due to its less invasive character (Helmberger et al. 2007). Nowadays, it is important to note that thermal ablation is already recognized as a curative modality (the other two curative modalities being surgical resection and transplantation) for hepatocellular carcinoma (HCC) per the BCLC (Barcelona Clinic Liver Cancer) Criteria that are widely endorsed by other scientific organizations including EASL, ESMO, and AASLD (Sag et al. 2016). However, even patients suffering from metastases within their liver—being no surgical candidates due to inoparability—show significant benefit regarding survival compared to those patients undergoing chemotherapy only. During the last 5 years, the acceptance of these thermal ablative therapies grew due to sound data especially in the treatment of CRC metastases (Gillams et al. 2015) and in 2016 thermal ablation was also included in the so-called “interventional toolbox” for limited liver metastases during the ESMO meeting (De Baere 2017; Van Cutsem et al. 2016). Due to the rapid growing acceptance for minimally invasive thermal therapy for liver malignancies, ablative therapies (especially radiofrequency ablation, now an increasing number of microwave ablations) are being more and more used for the treatment of extrahepatic tumors especially within the lung, kidney, and in bone in both curative (osteoid osteoma) and palliative (osteolyses) intention.
The aim of this chapter therefore is to describe technical details and the major applications. Furthermore, it will give a short summary of the latest literature—with an emphasis on RFA and especially RFA of the liver due to the widespread use of this technique and the clinically accepted indication for RF ablation of liver tumors.
2 Technique
By principle, there are different types of energy sources causing either heat (RFA, laser, Microwave) or cold (kryoablation) or high voltage (IRE) and therapies like ionizing radiation (stereotactic irradiation) or radiosurgery (Cyber-knife). While RFA and MWA are well known and used by many physicians, laser, IRE, and especially kryotherapy are used only by few centers, due to several drawbacks. All heating techniques have to raise tissue temperatures to a degree of at least 60–100° centigrade to cause sufficient coagulation necrosis while kryotherapy freezes cells to deaths using tissue temperatures below minus 20° centigrade.
2.1 Radiofrequency Ablation
The first experiments in thermal ablation of living tissue were described by d’Arsonval as early as 1868, while the use of thermal ablation for treatment of malignant hepatic lesions was first suggested by McGahan et al. and Rossi et al. in 1990 (Mcgahan et al. 1990). Radiofrequency ablation involves the delivery of high-frequency electrical current (375–480 kHz) into tissue causing cell death. There are two different types of RFA. In monopolar systems grounding electrodes have to be placed on the patient’s thighs or back to allow current conduction, while in bipolar or multipolar systems grounding pads are redundant as the electrical circuit is completed by either two electrodes or both mounted on a single needle (Mcgahan et al. 1996). This high frequency electrical current causes a rapid movement of ions within the tissue surrounding the electrode leading to frictional heat (Mcgahan et al. 1990). Reliable cell death only occurs, if the temperature exceeds 60 °C. However, temperatures of more than 105° are not as effective, due to possible carbonization and vaporization around the RF probe. The maximal achievable necrosis within tissue is not only dependent on tumor type and surrounding vessels but also on the shape of the electrode. Using needle-shaped electrodes, only tissue within a maximum diameter of 1.6 cm around the electrode can be destroyed. However, treatment of larger tumor volumes is possible with the development of different types of electrodes including mounting of additional needles in a cluster—arrangement or umbrella-shaped electrodes with a diameter of up to 7 cm (Goldberg 2001). Apart from tumor size and needle shape the effect of radiofrequency ablation and its completeness is also dependent on vascularization of the tumor and the surrounding tissue. Large vessels can cause the so-called “heat-sink effect”—describing the loss of temperature by cooling mediated by blood flow. This effect is well known especially in liver tumors and is most often caused by blood flow within branches of the portal vein, liver veins, or vena cava.
2.2 Microwave Ablation (MWA)
In contrast to Radiofrequency ablation—microwaves excite the electric dipoles of water molecules, which are forced to align with the rapidly alternating electric field, resulting in heat due to the friction of the rotating water molecules. Due to the physics behind the method, MWA needs no ions and no current conduction to heat the surrounding tissue. Therefore, boiling, charring, and vaporization in the close vicinity to the MWA antenna is no longer a problem during the delivery of the energy needed to destroy the tumor (Brace 2009; Mahnken et al. 2013). The effect of MWA is described by permittivity, which varies widely from one tissue type to another and is even different between a metastases and healthy tissue within the same organ (Joines et al. 1994).
Due to its thermal properties reaching temperatures up to 180 °C at the tip of the antenna and a faster increase in temperature levels, there are some data existing which argue for a lower heat sink effect compared to RFA in the proximity of large vessels (e.g., liver veins, vena cava, portal vein) and therefore a more predictable ablation zone (Schramm et al. 2006, 2007). However, a reduction of local recurrence for metastases located close to large vessels has never been proven in clinical trials.
Another possible advantage over RFA is the possibility to activate several probes at the same time. The synergy of multiple antennas allows for larger ablation volumes that are nearly six times larger than those achieved with single antenna ablations.
2.3 Irreversible Electroporation
Irreversible electroporation (IRE) is a quite new tissue ablation technique in which electrical pulses are delivered to tumor tissue to produce cell necrosis. At a specific threshold of electric potential, the cell membrane lipid bilayer becomes inundated with pores causing an increase in cell membrane permeability when ultra-short electrical pulses (micro- to milliseconds) are applied across a cell. This increase in membrane permeability is associated with the formation of nanoscale defects—or pores in the cell membrane (Weaver 1995). Cell death is therefore caused by a loss of cells’ homeostatic mechanism and due to the loss of cell membrane integrity and not due to thermal effects.
Studies (Rubinsky 2007; Rubinsky et al. 2007) show that the IRE ablated area is completely necrotic with a very sharp margin to untreated tissue, which is several cell layers thick. Larger vascular structures remain intact and heat sink effect does not influence the result of IRE at all. Another possible benefit of this new technique is that connective tissue and collagen are not affected—and therefore harming bile ducts, nerves, or the collecting system of the kidneys no longer is an obstacle of percutaneous ablation. A major drawback of IRE is that the application of short periods of high voltage electrical pulses (up to 3 kV in the studies mentioned above) causes a significant muscle contraction which can be observed in patients. Furthermore the pulses have to be synchronized to the heart beat and have to be delivered during the refractory cardiac period to avoid serious dysrhythmias, arrhythmias, or even cardiac arrest caused by the applicated electrical pulses. Therefore it is mandatory to do the IRE only under general anesthesia with complete muscle relaxation and together with a very experienced anestiologist.
IRE has been used clinically mainly in the liver, pancreas, kidney, and lung, while new applications are emerging for the prostate and even for eye or brain (Silk et al. 2014).
Up to now, IRE is an exciting new modality that can extend patient care to those with contraindications for thermal ablation; however more studies are needed to optimize device settings, probe positioning, and treatment parameters. Especially in scenarios where sensitive surrounding structures or major blood vessels are present, IRE can already be used to extend the armamentarium of interventional oncology.
2.4 Laser
Actually, there are two types of laser commercially available for image-guided laser ablation. Both types of laser (NdYAG with a wavelength of 1064 nm and solid state laser with a wave length of 805 nm) use photon absorption and heat conduction to create tissue heating and therefore a coagulation necrosis comparable to the effect of radiofrequency ablation. The laser energy is delivered via flexible laser fibers with diameters between 400 and 600 μm. While the point source at the tip of the bare laser fiber creates a more roundish necrosis, the fibers with diffuser technique are creating a more elliptic lesion. A possible advantage of laser ablation is a more predictable size and shape of the achievable necrosis. However, compared to RF ablation, drawbacks of this technique are higher costs and the more invasive approach especially in larger tumors due to the necessity for multiple fibers and therefore multiple introducer sheaths.
2.5 Kryoablation
Cryotherapy uses liquid nitrogen and argon gas via cryoprobes as coolants to produce temperatures below −20° centigrade. By repetitive freezing and thawing of the targeted tissue around the cryoprobe a predictable thermal necrosis is achieved. While the major disadvantage of the prior used probes was the large size and therefore the need for laparoscopic approach has been overcome by the newly developed smaller probes, cryotherapy is said to cause more complications due to the missing coagulation of vessels and therefore the higher risk of bleeding compared to RF. The possibility to monitor the development of the ice ball using ultrasound or MRI with an accuracy of 1–5 mm could be an advantage with respect to a higher rate of complete tumor ablation.
3 Clinical Applications
3.1 Primary and Secondary Liver Tumors
In most patients with a history of cancer, liver metastases occur—depending on the tumor—in up to 70%. These metastases have the highest impact on patient’s long-term survival and are responsible for the largest part of cancer-related deaths worldwide (Tranberg 2004). In Europe and the USA metastases of colorectal cancer and breast cancer is the most common indication for liver resection. Successful resection has a significant impact on the 3-, 5-, and 10-year survival rate published to be as high as 45%, 30%, and 20%, respectively (Scheele et al. 1995). Therefore, surgical resection is still considered to be the gold standard in liver metastases, while chemotherapy and radiation therapy are seen as palliative treatment options. However, due to risk factors only 10–25% of all patients suffering from liver metastases are suitable candidates for liver surgery. And—in spite of new chemotherapeutic options—the number of resectable patients is without a significant improvement during the last 20 years (Clark and Smith 2014). This has a major impact on the demand for minimally invasive treatments achieving an effective and reproducible percutaneous tumor ablation while simultaneously lowering both morbidity and costs.
3.1.1 Indications and Contraindications
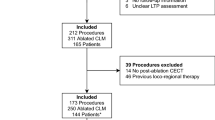
The indications for local ablative treatment are comparable to those established for resection—however with some modifications (Table 1). RFA is indicated for patients suffering from unresectable metastases due to tumorspread in both liver lobes or due to contraindications to surgical treatment or, according to the ESMO guidelines, even as an alternative therapy to surgery in patients after a successful induction chemotherapy. The combination of RFA with surgical resection as an adjuvant therapy or as a neoadjuvant therapy for bi-lobar tumors is also an accepted indication. Most investigators have limited ablative treatment to patients with four or fewer hepatic tumors with a diameter of 4–5 cm or smaller due to a significantly higher local recurrence rate in tumors larger than 3 cm (Curley et al. 1999; Curley et al. 2000). Ideally, tumors are smaller than 3.5 cm in diameter and completely surrounded by hepatic parenchyma, with a distance of at least 1 cm to the liver capsule and of more than 2 cm to the large hepatic or portal veins. Contraindications include extrahepatic spread of the tumor, a tumor volume of more than 30% of the total liver volume, sepsis, and uncorrectable coagulopathies (Curley 2003). Additionally, tumor location next to the large portal triads is a relative contraindication due to the risk of harming the bile duct. Subcapsular liver tumors can be treated with RFA; however, the treatment is usually associated with greater procedural and postprocedural pain and often associated with a higher complication rate (Lencioni and Crocetti 2005). Furthermore, tumors larger than 3–4 cm can be treated, using newer RF generators, multiple needle positions, or angiographically assisted RFA, however with a higher local recurrence rate (Sag et al. 2016). Tumors adjacent to large blood vessels are more difficult to treat because perfusion mediated tissue cooling reduces the extent of coagulation necrosis produced by thermal ablation. The blood flow mediated heat sink effect protects the vascular endothelium from thermal injury, allowing the placement of the electrodes as close as necessary to the vessels (Fig. 1).
(a–c) 25-year-old male patient with a history of a neuroendocrine tumor of the pancreas has developed a solitary liver metastasis. Patient was treated according to the local tumor board. (a) shows the hypervascularized lesion located in segment 7 of the liver. Control scan (b) immediately after the ablation with the needle still in place showing a successful ablation confirmed in the scan 24 h after treatment (c)
3.1.2 Results in Liver Metastases
In the early 2000, only few studies existed with good long-term follow evaluating local recurrence, disease-free survival, and overall survival after ablation. However, proof exists that completeness of tumor ablation is directly related to survival (Ahmad et al. 2006), comparable to a free resection margin after surgery (Scheele et al. 1995). Moreover, the local recurrence rate significantly depends on the size of the treated metastases (Curley 2003; Solbiati et al. 2001; Wood et al. 2000). In the study by CURLEY (Curley 2003) a local relapse in only about 7% of the patients was shown after RFA of colorectal metastases—however 80% of the local recurrences developed in the periphery of tumors larger than 5 cm in diameter.
De Baere and colleagues (Elias et al. 2000) analyzed 68 patients with 121 hepatic metastases who underwent 76 sessions of RFA with or without additional surgery. 47 patients with 88 metastases ranging from 1 to 4.2 cm in diameter were treated with RFA alone while the remaining 21 patients underwent a combination of surgery and intraoperative RFA for remaining small tumors. In 33 patients with 67 metastases who underwent percutaneous RFA a follow-up of at least 4 months was available, showing a local relapse in only 10% of the lesions (21% of the patients). A mean follow-up of 13.7 months was available for all patients showing 79% of the patients treated with percutaneous RFA were alive, 42% had no evidence of new or recurrent malignant hepatic disease, but only 27% were completely tumor free (Elias et al. 2000). A study published by GILLAMS et al. (Gillams and Lees 2004) referred on a cohort of 167 patients with colorectal liver metastases treated with percutaneous RFA. The authors were able to show a median survival period of 38 months, with a 5-year survival rate of 30% after the diagnosis of liver metastases. Furthermore, a survival period of 31 months, with a 5-year survival rate of 25%, after the first ablation was reported. The authors concluded from their results that RFA increases the therapeutic options for patients with colorectal metastases.
Since then multiple studies were published on this topic—and 16 studies with a high scientific quality were summarized in the position paper by A. Gillams (Gillams et al. 2015). In this review paper 1613 patients with surgically untreatable tumors were summarized. In these patients the mean number of tumors was 2.2 and the mean tumor size was 2.6 cm. Mean 3-year and 5-year survival was 50% (37–77%) and 31% (17–51%), respectively. Furthermore in this position paper was stated that thermal ablation is particularly effective in treating small to mid-size metastases. The expert panel figured out that the common cutoff is 3 cm—however—depending on the anatomically location of the metastases—even tumors with a diameter of up to 5 cm can be completely eradicated. The recurrence rate of tumors with a size of more than 5 cm is reported to be as high as 27–45%—and therefore RFA is not recommended in a curative intent. And even in the “first line” RFA can be successfully used in primarily resectable patients with metastases smaller than 3 cm with the same 3-year survival rate—as published by Otto et al. (Otto et al. 2010).
Another more recent review by Petre and Sofocleous (Petre and Sofocleous 2017) focusing on recent studies reporting on the safety, efficacy, and long-term outcomes of different thermal ablative therapies gives a very elaborated overview. In their publication they stated that there is growing evidence in the reviewed literature, that proofs that RFA in small metastases is able to provide similar results like surgery. The critical size for metastases seems to be 3 cm—with a significant increase in local relapse if this diameter is not respected. Furthermore they stated as major advantages that thermal ablation can be repeated to treat an additional progress, does not impact surgical eligibility for those which can be resected in the future, does not need a prolonged chemotherapy interruption, and last but not least maintains patient’s quality of life.
A remaining question is which technique to use—RFA or MWA. To answer this question there are only few studies comparing both studies. A quite recent study (Huo and Eslick 2015) published in 2015 reviewed 10 prospective and 6 retrospective studies evaluating MWA and RFA treatment outcomes in patients with primary and metastatic liver tumors. This review was able to prove a benefit for MWA regarding the 6-year survival but no difference in overall recurrence rate and complete ablation. However, there was a benefit for patients undergoing MWA regarding local recurrence.
3.1.3 Results in HCC
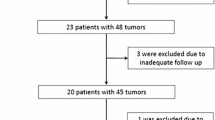
Ablative treatment concepts represents nowadays the first line option in the early stage (unresectable) HCC. Beside the primary treatment in curative intent thermal ablation is a widely accepted tool in the bridging/downstaging concept before liver transplantation. Treatment success varies in HCC with the size of the lesion to be treated comparable to that of metastases as described above. The reported experience of Buscarinietal (Buscarini et al. 2001) in 88 patients showed that complete tumor necrosis is only achievable in tumors smaller than 3.5 cm in maximum diameter. Similar results were shown in a review by Poon (Poon et al. 2002) in which a complete tumor necrosis was achieved in 80–90% of tumors smaller than 3–5 cm in size after a single treatment session.
A prospective clinical trial performed on 187 patients showed promising results concerning long-term survival in HCC patients after RFA (Lencioni et al. 2005). Overall survival rates were 97% at 1 year, 89% at 2 years, 71% at 3 years, 57% at 4 years, and 48% at 5 years follow-up. The survival rates of patients with a Child-Pugh class A cirrhosis (n = 144; 76% at 3 years and 51% at 5 years) were significantly higher than those of patients with a Child-Pugh class B cirrhosis (n = 43; 46% at 3 years and 31% at 5 years). The data published by Tateishi et al. (Tateishi et al. 2005) concerning percutaneous RF-ablation of HCC in 664 patients are also very encouraging. The authors assessed the cumulative survival in patients who received RFA as the primary treatment (n = 319, naïve patients) as well as in patients who received RFA for recurrent tumor (n = 345, non-naïve patients) after previous treatment including surgical resection, microwave coagulation therapy, PEI, and TACE. The cumulative survival rates at 1, 2, 3, 4, and 5 years were 94.7%, 86.1%, 77.7%, 67.4%, and 54.3% for naive patients, whereas the cumulative survival rates were 91.8%, 75.6%, 62.4%, 53.7%, and 38.2% for non-naive patients, respectively.
In the last few years, even 10 years data were published by different groups (Kim et al. 2013; Shiina et al. 2012). These data from China were as high as 27–32% and were concordant with the results from western groups (Facciorusso et al. 2016). Beside local tumor control there are different predictors of survival—namely liver function (Child Pugh scores) initial response, serum ferritin, number and size of nodules, and AFP levels (Facciorusso et al. 2014; Facciorusso et al. 2016; Lee et al. 2014) which have to be taken into account in the treatment and for the indication of thermal ablation.
Beside the clinical data—RFA seems to be not only equal to surgery in terms of overall survival but also more cost-effective compared to liver resection for early HCC (single nodule smaller than 2 cm) and even in the presence of two to three nodules less than 3 cm in diameter (Facciorusso et al. 2016).
3.1.4 Complications and Side Effects
The largest study regarding complications after radiofrequency ablation was published by LIVRAGHI et al. (Livraghi 2003) and reported the complication rates after treating 2320 patients with a total number of 3554 lesions. Six deaths (0.3%) were noted, including two fatalities caused by multiorgan failure following intestinal perforation. Furthermore, only 2.0.2% of all patients suffered from major complications with the most frequently observed complications being peritoneal hemorrhage, intrahepatic abscess formation, and intestinal perforation, while tumor seeding along the needle tract has been a rare complication as a track-ablation was performed after every thermal ablation (Livraghi 2001). Risk factors for peritoneal hemorrhage were superficial metastases, whereas intrahepatic abscesses were mostly observed in diabetic patients without periprocedural antibiosis. Furthermore, thermal damage to adjacent organs (colon, stomach) has rarely been described (Livraghi 2003). Minor complications, including post-ablation syndromes like post- or periprocedural pain, fever, and asymptomatic pleural effusion, were observed in less than 5% of patients. Pleural effusion can be detected regularly, especially after using an intercostal approach. Furthermore, the authors (Livraghi 2003) reported the rate of complications to be directly related to the number of required RF sessions. These results confirmed—in accordance with the experience of other authors—RFA to be a relatively low-risk procedure for the treatment of focal liver tumors (Curley et al. 2004; Liu et al. 2002; Mulier et al. 2002; Pereira et al. 2003).
3.2 Renal Cell Carcinoma
Small renal masses are commonly diagnosed incidentally. The majority are malignant in require treatment. CT-guided radiofrequency ablation as a minimally invasive therapy also shows promising results in the treatment of these small renal masses. However, there is still insufficient data regarding long-term outcome after RFA (Fig. 2).
Therefore, partial nephrectomy and nephron sparing surgery is considered to be gold standard for the treatment of renal cell carcinoma. However, even in very experienced centers complication rate is described to be up to 30% (Haber and Gill 2006) after laparoscopic surgery with a notable amount (up to 2%) of renal insufficiencies. In comparison, the complication rate is very low in patients treated with RFA and major complications are described to be 2.2% as a maximum. Other authors published their data on 82 RF cases were not able to show significant impact on renal function measured by mean serum creatinine level. A multi-institutional study of 163 ablations with a follow-up of 18 months showed a recurrence-free survival of 92% (Gupta et al. 2009). Furthermore, partial nephrectomy or nephron sparing surgery has to be performed under general anesthesia, while RFA can be performed under conscious sedation in most of the cases—enabling even patients with severe comorbidities to undergo this type of treatment. In tumors larger than 5 cm, however, results are quite poor. Furthermore, there are no randomized controlled trials comparing thermal ablation against partial nephrectomy.
Due to the higher probability to develop a second tumor in the contralateral kidney after having suffered a RCC, these particular patients have to undergo regularly follow-up examinations. If tumors are detected in the follow-up, they are usually small. Especially in tumors smaller than 3 cm the success rate of RFA is nearly 100%. RFA requires less time and recovery, a shorter hospitalization, reduced pain, morbidity and mortality in comparison to more invasive surgical methods (Mouraviev et al. 2007) and is even less expensive compared to traditional methods (Lotan and Cadeddu 2005).
3.3 Lung Tumors
Radiofrequency ablation can also be used for the treatment of small primary and secondary tumors located in the lung. Several hundred procedures have been performed and published worldwide showing very good results at reasonable low complication rates. The overall pneumothorax rate is similar to that of CT-guided percutaneous lung biopsies ranging between 20 and 40% with less than 20% requiring a drainage insertion (Hoffmann et al. 2006; Kelekis et al. 2006). Ideal tumors for RF treatment are smaller than 3 cm in diameter, located in the periphery and should have a distance of at least 1 cm to large pulmonary vessels or bronchi. Furthermore, the number of tumors within each lung should not exceed 3 and patients should not qualify for open surgery. For probe positioning the use of CT together with CT fluoroscopy is recommended. However, there is no recommendation whether the therapy should be done under general anesthesia or conscious sedation but there is proof that there is no difference in using either of them (Hoffmann et al. 2006). A successful ablated tumor shows no further contrast enhancement and a ground glass shadowing completely surrounding the tumor. Furthermore, ablated lung tumors seem to increase in size after 3 months due to necrosis of healthy surrounding tissue but normally show significant shrinkage after 6 and 12 months due to progressive scarring (Fig. 3).
(a–c) 55-year-old male patient with a solitary pulmonary metastasis due to colorectal cancer. Patient did not want to undergo open surgery, therefore RF ablation was performed using CT fluoroscopic guidance (b) Control scan (c) 24 h after treatment showed no complication and the lesion completely covered as indicated by the ground glass opacities surrounding the metastasis
A recent review by de Baere and colleagues included 17 reports of lung RFA for NSCLC and showed the median complete ablation being as high as 90%, with tumors smaller than 2 cm have a complete ablation rate of up to 98% (De Baere et al. 2016). In this review the highest 1-, 3-, and 5-year survival rates were reported to be 97.7%, 72.9%, and 55.7%. Another study by de Baere et al. (De Baere et al. 2015) included 566 patients with more than 1000 metastases treated. Four-year local efficacy was 89% and the 4-year lung disease control rate was 44.1%, with patient retreated safely up to four times. Primary origin, disease-free interval, size, and number of metastases were associated with OS in multivariate analysis (De Baere et al. 2015).
However, until now, the results published in literature regarding technical feasibility, therapeutic response, and short-term survival (Kelekis et al. 2006) are encouraging, but there is still too less proof so far for a clinical benefit in the long-term follow-up.
3.4 Bone and Soft Tissue Tumors
Radiofrequency ablation in the treatment of benign osteoid osteoma causing severe pain is a well known and clinically accepted indication and has replaced open surgery due to its less invasive character and higher success rate regarding clinical symptoms (Woertler et al. 2001).
Especially in palliative situations radiofrequency ablation has successfully been applied to osteolytic metastases and soft tissue tumors involving the bone to relief pain (Goetz et al. 2004) or as an adjunct to vertebro—or osteoplasty. Furthermore, RFA has also been used for tumor debulking, if the tumor causes pressure symptoms like dysphagia or dyspnea.
Conclusion
Percutaneous thermal ablation therapies have been receiving increasing attention as a potential primary treatment for focal HCC and liver metastases. Possible advantages of ablative therapies as compared to surgical resection include a lower morbidity and mortality rate, lower costs, the suitability for real-time imaging guidance, the option to perform ablative procedures on outpatients, and the potential application to a wider spectrum of patients, including those who are unsuitable as surgical candidates. Therefore, the major advantage of RFA is its ability to create a well-controlled focal thermal injury in the liver resulting in high success rates in treating HCC nodules and metastases smaller than 3 cm in diameter with long-term results comparable to surgery.
Beside the accepted application of thermal ablation in patients suffering from liver tumors, RFA has a rapidly growing role in tumors beyond the liver. Especially in renal and lung cancer RF ablation shows very promising results, however, larger studies are still missing proofing its effectiveness regarding the long-term follow-up.
References
Ahmad A, Chen SL, Kavanagh MA et al (2006) Radiofrequency ablation of hepatic metastases from colorectal cancer: are newer generation probes better? Am Surg 72:875–879
Brace CL (2009) Radiofrequency and microwave ablation of the liver, lung, kidney, and bone: what are the differences? Curr Probl Diagn Radiol 38:135–143
Buscarini L, Buscarini E, Di Stasi M et al (2001) Percutaneous radiofrequency ablation of small hepatocellular carcinoma: long-term results. Eur Radiol 11:914–921
Clark ME, Smith RR (2014) Liver-directed therapies in metastatic colorectal cancer. J Gastrointest Oncol 5:374–387
Curley SA (2003) Radiofrequency ablation of malignant liver tumors. Ann Surg Oncol 10:338–347
Curley SA, Izzo F, Delrio P et al (1999) Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg 230:1–8
Curley SA, Izzo F, Ellis LM et al (2000) Radiofrequency ablation of hepatocellular cancer in 110 patients with cirrhosis. Ann Surg 232:381–391
Curley SA, Marra P, Beaty K et al (2004) Early and late complications after radiofrequency ablation of malignant liver tumors in 608 patients. Ann Surg 239:450–458
De Baere T (2017) The IR evolution in oncology: tools, treatments, and guidelines. Cardiovasc Intervent Radiol 40:3–8
De Baere T, Auperin A, Deschamps F et al (2015) Radiofrequency ablation is a valid treatment option for lung metastases: experience in 566 patients with 1037 metastases. Ann Oncol 26:987–991
De Baere T, Tselikas L, Catena V et al (2016) Percutaneous thermal ablation of primary lung cancer. Diagn Interv Imaging 97:1019–1024
Elias D, Goharin A, El Otmany A et al (2000) Usefulness of intraoperative radiofrequency thermoablation of liver tumours associated or not with hepatectomy. Eur J Surg Oncol 26:763–769
Facciorusso A, Del Prete V, Antonino M et al (2014) Serum ferritin as a new prognostic factor in hepatocellular carcinoma patients treated with radiofrequency ablation. J Gastroenterol Hepatol 29:1905–1910
Facciorusso A, Serviddio G, Muscatiello N (2016) Local ablative treatments for hepatocellular carcinoma: an updated review. World J Gastrointest Pharmacol Ther 7:477–489
Gillams A, Goldberg N, Ahmed M et al (2015) Thermal ablation of colorectal liver metastases: a position paper by an international panel of ablation experts, the interventional oncology sans frontieres meeting 2013. Eur Radiol 25:3438–3454
Gillams AR, Lees WR (2004) Radio-frequency ablation of colorectal liver metastases in 167 patients. Eur Radiol 14:2261–2267
Goetz MP, Callstrom MR, Charboneau JW et al (2004) Percutaneous image-guided radiofrequency ablation of painful metastases involving bone: a multicenter study. J Clin Oncol 22:300–306
Goldberg SN (2001) Radiofrequency tumor ablation: principles and techniques. Eur J Ultrasound 13:129–147
Gupta A, Raman JD, Leveillee RJ et al (2009) General anesthesia and contrast-enhanced computed tomography to optimize renal percutaneous radiofrequency ablation: multi-institutional intermediate-term results. J Endourol 23:1099–1105
Haber GP, Gill IS (2006) Laparoscopic partial nephrectomy: contemporary technique and outcomes. Eur Urol 49:660–665
Helmberger T, Dogan S, Straub G et al (2007) Liver resection or combined chemoembolization and radiofrequency ablation improve survival in patients with hepatocellular carcinoma. Digestion 75:104–112
Hoffmann RT, Jakobs TF, Lubienski A et al (2006) Percutaneous radiofrequency ablation of pulmonary tumors—is there a difference between treatment under general anaesthesia and under conscious sedation? Eur J Radiol 59:168–174
Huo YR, Eslick GD (2015) Microwave ablation compared to radiofrequency ablation for hepatic lesions: a meta-analysis. J Vasc Interv Radiol 26:1139–1146e1132
Joines WT, Zhang Y, Li C et al (1994) The measured electrical properties of normal and malignant human tissues from 50 to 900 MHz. Med Phys 21:547–550
Kelekis AD, Thanos L, Mylona S et al (2006) Percutaneous radiofrequency ablation of lung tumors with expandable needle electrodes: current status. Eur Radiol 16:2471–2482
Kim YS, Lim HK, Rhim H et al (2013) Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: analysis of prognostic factors. J Hepatol 58:89–97
Lee DH, Lee JM, Lee JY et al (2014) Radiofrequency ablation of hepatocellular carcinoma as first-line treatment: long-term results and prognostic factors in 162 patients with cirrhosis. Radiology 270:900–909
Lencioni R, Crocetti L (2005) A critical appraisal of the literature on local ablative therapies for hepatocellular carcinoma. Clin Liver Dis 9:301–314, viii
Lencioni R, Della Pina C, Bartolozzi C (2005) Percutaneous image-guided radiofrequency ablation in the therapeutic management of hepatocellular carcinoma. Abdom Imaging 30:401–408
Liu LX, Jiang HC, Piao DX (2002) Radiofrequence ablation of liver cancers. World J Gastroenterol 8:393–399
Livraghi T (2001) Guidelines for treatment of liver cancer. Eur J Ultrasound 13:167–176
Livraghi T (2003) Radiofrequency ablation, PEIT, and TACE for hepatocellular carcinoma. J Hepato-Biliary-Pancreat Surg 10:67–76
Lotan Y, Cadeddu JA (2005) A cost comparison of nephron-sparing surgical techniques for renal tumour. BJU Int 95:1039–1042
Mahnken AH, Pereira PL, De Baere T (2013) Interventional oncologic approaches to liver metastases. Radiology 266:407–430
Mcgahan JP, Browning PD, Brock JM et al (1990) Hepatic ablation using radiofrequency electrocautery. Investig Radiol 25:267–270
Mcgahan JP, WZ G, Brock JM et al (1996) Hepatic ablation using bipolar radiofrequency electrocautery. Acad Radiol 3:418–422
Mouraviev V, Joniau S, Van Poppel H et al (2007) Current status of minimally invasive ablative techniques in the treatment of small renal tumours. Eur Urol 51:328–336
Mulier S, Mulier P, Ni Y et al (2002) Complications of radiofrequency coagulation of liver tumours. Br J Surg 89:1206–1222
Otto G, Duber C, Hoppe-Lotichius M et al (2010) Radiofrequency ablation as first-line treatment in patients with early colorectal liver metastases amenable to surgery. Ann Surg 251:796–803
Pereira PL, Trubenbach J, Schmidt D (2003) Radiofrequency ablation: basic principles, techniques and challenges. Rofo 175:20–27
Petre EN, Sofocleous C (2017) Thermal ablation in the management of colorectal cancer patients with oligometastatic liver disease. Visc Med 33:62–68
Poon RT, Fan ST, Tsang FH et al (2002) Locoregional therapies for hepatocellular carcinoma: a critical review from the surgeon’s perspective. Ann Surg 235:466–486
Rubinsky B (2007) Irreversible electroporation in medicine. Technol Cancer Res Treat 6:255–260
Rubinsky B, Onik G, Mikus P (2007) Irreversible electroporation: a new ablation modality—clinical implications. Technol Cancer Res Treat 6:37–48
Sag AA, Selcukbiricik F, Mandel NM (2016) Evidence-based medical oncology and interventional radiology paradigms for liver-dominant colorectal cancer metastases. World J Gastroenterol 22:3127–3149
Scheele J, Stang R, Altendorf-Hofmann A et al (1995) Resection of colorectal liver metastases. World J Surg 19:59–71
Schramm W, Yang D, Haemmerich D (2006) Contribution of direct heating, thermal conduction and perfusion during radiofrequency and microwave ablation. Conf Proc IEEE Eng Med Biol Soc 1:5013–5016
Schramm W, Yang D, Wood BJ et al (2007) Contribution of direct heating, thermal conduction and perfusion during radiofrequency and microwave ablation. Open Biomed Eng J 1:47–52
Shiina S, Tateishi R, Arano T et al (2012) Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol 107:569–577; quiz 578
Silk M, Tahour D, Srimathveeravalli G et al (2014) The state of irreversible electroporation in interventional oncology. Semin Intervent Radiol 31:111–117
Solbiati L, Ierace T, Tonolini M et al (2001) Radiofrequency thermal ablation of hepatic metastases. Eur J Ultrasound 13:149–158
Tateishi R, Shiina S, Teratani T et al (2005) Percutaneous radiofrequency ablation for hepatocellular carcinoma. An analysis of 1000 cases. Cancer 103:1201–1209
Tranberg KG (2004) Percutaneous ablation of liver tumours. Best Pract Res Clin Gastroenterol 18:125–145
Van Cutsem E, Cervantes A, Adam R et al (2016) ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol 27:1386–1422
Weaver JC (1995) Electroporation theory. Concepts and mechanisms. Methods Mol Biol 55:3–28
Woertler K, Vestring T, Boettner F et al (2001) Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol 12:717–722
Wood TF, Rose DM, Chung M et al (2000) Radiofrequency ablation of 231 unresectable hepatic tumors: indications, limitations, and complications. Ann Surg Oncol 7:593–600
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Hoffmann, RT. (2017). CT-Guided Tumor Ablation. In: Nikolaou, K., Bamberg, F., Laghi, A., Rubin, G.D. (eds) Multislice CT. Medical Radiology(). Springer, Cham. https://doi.org/10.1007/174_2017_155
Download citation
DOI: https://doi.org/10.1007/174_2017_155
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42585-6
Online ISBN: 978-3-319-42586-3
eBook Packages: MedicineMedicine (R0)