Abstract
Thoracic trauma is the most common injury in polytrauma patients, with an incidence rate of 45–65%, and the most common cause of trauma deaths (about 20 % of all deaths), second only to head injuries.
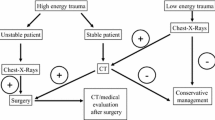
In the time-sensitive acute care setting, efficiency and rapidity are basic. The Chest-X-Ray (CXR) may be considered as an adjunct to the initial assessment or primary survey of unstable traumatic patients. It helps to identify a tension pneumothorax (PNX) and pleural effusions that may suggest a hemothorax, until further evidence.
MultiSlice Computed Tomography (MSCT) is always the last step of the diagnostic procedures for stable patients, regardless of the positive or negative results on CXR, being the gold standard for the radiologic evaluation of the chest in traumatic patients.
This chapter will review the wide spectrum of radiographic and MSCT findings in patients undergoing a thoracic trauma, both blunt and penetrating, with a particular focus on the role of the radiologist in the management of major trauma, together with the “trauma team”.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
1.1 Epidemiology and Mechanism of Injury
Thoracic trauma is the most frequent injury in polytrauma patients, with an incidence rate of 45–65 %, second only to head injuries. Even though some mechanisms of injury may result in thoracic penetrating trauma from sharp objects, thoracic trauma is more often due to high-energy blunt trauma, with a mortality rate approaching 60 %. According to some statistics, thoracic trauma represents the most common cause of trauma deaths (about 20 % of all deaths), next to head trauma (Gaillard M 1990).
Among the causes of a high-energy blunt trauma (high-height falls, workplace accidents, etc.), traffic accidents account for 70–80 % of the patients; moreover, one-third of hospitalized patients following a traffic accident may present signs of major thoracic trauma.
Several studies have shown that, when a car crash occurs, passengers wearing a seat belt may sustain significant thoracic injuries at a speed of at least 48 km/h, whereas unrestrained passengers may suffer severe injuries even at an impact speed of 16 km/h. Therefore, a lot of authors recommend the use of multi-slice computed tomography (MSCT), irrespective of the findings of the chest X-ray (CXR), supine anterior-posterior projection (AP view) of the thorax, to avoid ignoring potentially fatal chest injuries (Traub M et al 2007; Van Hise ML et al. 1998).
However, other authors have highlighted the importance of not underestimating falls from low heights, particularly in the aging population, to whom even minor trauma may be fatal. The mechanisms of injury of pleuro-parenchymal traumas will be treated in the sections concerning the different types of injuries: here, it is only pointed out that the elastic characteristics of the chest wall, particularly in infants and young children, can frequently result in the presence of significant pleuro-parenchymal injuries (e.g., hemopneumothorax) associated with an intact rib cage (about ¼ of cases).
As regards lungs and abdominal organs, it is available a scientific and clinical classification, an injury grading system from the American Association for the Surgery of Trauma (AAST). However, this injury scale will not be reported in this study, because there is not much literature available.
1.2 The Role of the Radiologist
The radiologist should always play a central role in the management of major traumas (Injury Severity Score >15), together with the “trauma team” (surgeon, anesthetist, nursing staff, and radiographers). Moreover, the radiologist should be familiar with the general principles of the state-of-the-art clinical polytrauma management that in many institutions is based on the Advanced Trauma Life Support (ATLS) protocols (periodically updated) from the American College of Surgeons Committee on Trauma. Nevertheless, it is not stated that the role of the radiologist involved in the polytrauma management is unquestionably that provided by the ATLS protocols, but that a sound knowledge of the general ATLS principles is essential to have full awareness of his clinical role: only such “self-awareness” will allow him to express himself to the best as well as to defend himself from undue and unfounded demands.
For the radiologist, the key principles of ATLS are probably two: “treat first that kills first” and “imaging should not intervene with or postpone treatment.” Ultimately, this means that any condition that threatens airway, breathing, circulation, and disability (ABCD) is to be treated according to priorities for the immediate patient survival, using diagnostic imaging if and when very appropriate, however, never before the stabilization of the patient’s vital signs, knowing that “the lack of a definitive diagnosis should never delay an indicated treatment.” (Mayberry JC et al. 2000)
In the following chapter, only limited to consider lungs and pleura, it is suggested that, when an appropriate radiological assessment is obtained, the radiologist has to evaluate the findings according to the well-known priorities ABC: airway, breathing, and circulation. Regarding the pleura and lung parenchyma, there are two diagnostic high priorities: tension pneumothorax and bleeding, particularly active bleeding within the parenchyma and the pleural space (pulmonary hematoma and hemothorax).
In brief: obtaining diagnostic assessments according to ABCD priorities and evaluating images according to the same ABCD priorities.
1.3 Diagnostic Imaging
In the emergency setting, the CXR, anteroposterior radiogram of the thorax, acquired with the patient in clinostasis, may be considered as an adjunct to the initial assessment or primary survey of trauma patients. An appropriate diagnostic imaging cannot interfere with the resuscitation process and, if necessary, can and has to be postponed until the secondary survey.
According to some authors, in the initial assessment of trauma patients, CXR should be done together with the cervical rachis and pelvis X-ray: it should be performed only on unstable patients as well as on patients with abnormal findings on chest examination.
Regarding the pleura and lung assessment, the first aim of a radiologist performing a CXR is to inspect for evidence of a tension pneumothorax (PNX) and pleural effusions that may suggest a hemothorax, until further evidence (Ianniello S et al. 2014). The diagnosis of hematoma is difficult, and the differential diagnosis for parenchymal contusion essentially remains a prerogative of MSCT. (Peters S et al. 2010; Rivas LA et al 2003)
MSCT is always performed in the secondary survey of the trauma patients; it is only addressed to hemodynamically stable patients or to patients already stabilized by the trauma team.
An unstable patient should not be moved in an MSCT suite in life-threatening conditions. Diagnostic assessment should be obtained simultaneously with the appropriate therapeutic procedures during the exploratory laparotomy and/or thoracotomy. When the patient’s clinical conditions require an immediate surgical intervention, CXR closes the chest preoperative diagnostic procedures (further assessments are postponed to potential postoperative MSCT follow-up), remaining, moreover, the imaging modality of choice for subsequent assessments. (Roy-Choudhury SH et al. 2007; Ryan MF et al. 2004).
On the contrary, after the trauma team has obtained the patient’s stabilization, it is necessary to continue with a second, more accurate diagnostic assessment (secondary survey) to be performed on MSCT (Miele V et al. 2015).
Stabilized patients, with normal physical examination for thoracic injury, should undergo a MSCT scan, regardless the findings on CXR. It has been proved that 39–50 % of trauma patients with unremarkable CXR may present multiple lesions on CT scan, leading to a change in the therapeutic management in 5 % of cases; on the other hand, trauma patients with remarkable CXR present further lesions on CT in the 66 % of cases, resulting in a treatment change in 20 % of cases.
In a recent population-based survey of patients admitted to ED following a high-energy trauma (such as falls from a height exceeding 3 m; traffic accidents at a speed higher than 50 km/h; ejections from the vehicle; vehicle rollovers; severe deformity of the passenger compartment; pedestrian accidents >10 km/h; bicycle collisions at a speed higher than 30 km/h; crush injury), the findings on a routine chest MSCT (even with unremarkable chest X-ray as well as normal physical examination) have allowed to diagnose additional findings in 43 % of the patients, compared with the conventional chest radiography, and have required a change in the management in 17 % of all patients.
Finally, some authors suggest to directly perform MSCT, which is by far more accurate in the detection of silent but potentially life-threatening clinical findings on stable patients with normal chest examination (such as small flaps of pneumothoraces, which in case of following intubation can lead to tension PNX).
With regard to the penetrating trauma, the previously stated principles are valid, but with a distinction: even if pneumothorax and hemothorax may be diagnosed on CXR, the MSCT screening is strictly recommended even in patients with an unremarkable CXR, in order to rule them out. Furthermore, patients with penetrating thoracic injuries may be likely to suffer abdominal injuries, until further evidence (Scaglione M et al. 2008; Scott et al. 2015; Sivit CJ et al. 1989).
In brief: the diagnostic procedures of the thorax for unstable patients finish with the execution of CXR, as part of the primary survey; the execution of MSCT is always the last step of the diagnostic procedures for stable patients, regardless of the positive or negative results on CXR. Some authors suggest the immediate execution of MSCT scan in stable patients presenting normal thoracic examination; but, according to the standard practice of many institutions, the CXR comes before MSCT anyway.
2 Pulmonary Contusion
Pulmonary contusion is the most common parenchymal lung injury seen in blunt thoracic trauma, with a prevalence of 30–75 % of cases. Pulmonary contusion is a hemorrhagic-edematous focal deposit, suggestive of a damage to the capillary-alveolar membrane, in the alveolar and interstitial space. The parenchymal architecture remains overall intact, even if associated parenchymal lacerations can be sometimes detected within the areas of contusion (Cohn SM 1997; Shanmuganathan K et al. 1999; Wagner 1988).
The mechanism of injury of pulmonary contusion is represented by a direct trauma (contusion on the lung immediately adjacent to the area of impact) or by a contrecoup trauma (contusion at the site opposite the impact). In the setting of high-energy deceleration trauma (i.e., motor-vehicle accidents), alveoli are subjected to sudden frictional forces (shear stress) from the bronchovascular peduncles; direct trauma may disrupt pulmonary alveoli (pulmonary contusions associated with lacerations, as in the case of a fractured rib); and the transmitted kinetic energy may deposit locally at a liquid-gas interface such as air-blood relationship in pulmonary alveoli.
Clinical symptoms, which about 50 % of patients present, include hemoptysis (transudation of blood within the alveolar spaces and the airways), mild fever, tachypnea, hypoxia, bronchorrhea, and acute respiratory failure.
Reduced lung compliance, reduced ventilation per unit volume, and increased shunt fraction are typical signs of contused pulmonary areas; the thickening of the alveolar septa reduces the locoregional gas diffusion in the contused lung.
In severe pulmonary contusion, the local response to the injury has systemic consequences, being related to a rise of the bronchoalveolar lavage (BAL) protein as well as an increase in capillary permeability: macroscopic and microscopic alterations, increased polymorphonuclear cells (neutrophils) even within the uninjured lung tissue, as well as increased local and systemic complement levels.
Most severe contusions requiring mechanical ventilation are associated with severe rib cage injury, although they are not necessarily associated with rib or sternal fracture. In particular, flail chest, the most severe form of blunt chest wall injury with mortality rates of 10–20 %, is typically associated with significant pulmonary contusion. The diagnosis of contusion is associated with the deterioration in the prognosis, above all, in the pediatric population (Trindade LM et al. 2009).
A strong correlation exists between the size of the pulmonary contusions and the mortality rate as well as the comorbidities for ARDS or pneumonia. Mortality rate for lung contusion varies from 14 to 40 %, depending on the severity of the extension. It is important to underline that the actual extension of a contusion cannot be detected at the initial radiologic work-up but it may be evident by 72 h following injury.
2.1 Diagnostic Imaging
Parenchymal contusion is the most common cause of pulmonary opacity on CXR after blunt chest trauma, occurring in 30–75 % of patients.
Radiographically, pulmonary contusion presents as focal or multifocal areas of confluent “ground-glass” opacity (Figs. 1 and 2) or consolidation (Fig. 3). Contusions are not limited by segmental boundaries and are usually visible in the lung periphery adjacent to the area of direct trauma. If contusion does not reveal perifocal injury site associated with parenchymal laceration, its pattern appears homogeneous, without any cavitation. Contusions may not be radiographically visible within 6 h after the trauma; they may develop progressively within 24–72 h, when maximum conspicuity is reached. Finally, uncomplicated contusions may resolve gradually after 3–10 days: pulmonary opacities, which do not clear or increase within such a period, raise the suspicion of developing secondary infection or acute respiratory distress syndrome (ARDS).
CT is highly sensitive in detecting pulmonary contusions: in experimental models, CT can detect pulmonary contusion in 100 % of cases compared with 37.5 % by chest radiographs, and it provides an accurate detection of the extent of the injury. However, there is a possibility that pulmonary contusions only visible on CT are not clinically significant. The feature on CT is dependent on the injury severity: “ground-glass opacity” is indicative of a mainly interstitial damage with partial alveolar filling, whereas consolidation is indicative of a severe alveolar damage, often associated with lacerations.
2.2 Differential Diagnosis
It may manifest as pathology of the airspaces, and differential diagnosis considers aspiration, atelectasis, and pneumonia. They all may have identical radiographic findings. Radiographic features of atelectasis include triangular shape and signs associated with volume loss; those of laceration the cavitating pattern within the radiopaque area. Lack of contusion clearance within 7–8 days should raise the suspicion of either associated laceration, pneumonia, or ARDS.
Air bronchogram sign is rare because distal airways are usually filled with blood or edema.
3 Pulmonary Laceration
Pulmonary lacerations are evident tears in the lung parenchyma, usually resulting either from shearing stress forces, secondary to high-energy trauma, or from direct puncture, i.e., due to fractured rib fragments. They may be associated with contusions that should represent a minor parenchymal damage. Clinically, pulmonary lacerations may manifest as hemoptysis.
Multiple types of lacerations can be seen in the same injured parenchyma simultaneously. They are usually benign lesions, although some complications may arise: infection, bronchopleural fistula, enlargement and subsequent compression of the surrounding parenchyma, and hemorrhage.
3.1 Diagnostic Imaging
The radiographic findings are variable and can change after admission to ED in subsequent examinations. The elastic recoil properties of the surrounding lung parenchyma give a round shape to the lacerations that are often difficult to identify on CXR. The space created by the tissue disruption may be filled with air, blood (hematoma), or more often both air and blood, creating air-fluid levels. In the acute stage, the blood, collected in the laceration, shows up a well-defined homogenous opacity, with density of soft tissue. Lacerations, sometimes masked by associated pulmonary contusions, become clearly detectable on serial follow-up examination, thanks to the clearance of the contusions. Lacerations, in fact, become more visible days after the trauma, with the shrinking of the edema and the hemorrhage, both associated with contusion. On occasion, small and multiple lacerative lesions are visible within areas of parenchymal contusion, in the form of focal uniform density, with a “Swiss cheese appearance.” Within areas of contusion, the detection of round, homogeneously dense focuses, indicative of multiple hematomas, is not rare.
With time, the hematoma within the laceration resolves, and it is replaced with a round or oval air cavity, referred to as posttraumatic pneumatocele. The posttraumatic pneumatocele appears within few days from trauma, but, in some cases, it can be evident after months; its size is usually 2–5 cm.
The detection of pulmonary lacerations is highly sensitive on MSCT, and, consequently, a classification into four types is possible:
-
Type 1: it is the most common type, centrally located; it results from shearing stress forces, developed between the lung parenchyma and the tracheobronchial tree (Fig. 4).
-
Type 2: often seen as a tubular lesion in the lower lobes, resulting from a compression force of the parenchyma across the vertebral body (the spine) (Fig. 5).
-
Type 3: it is small, rounded, peripherally located, associated with rib fractures and a PNX (Fig. 6).
-
Type 4: it is a tear in the preexisting pleuropulmonary adhesions; it is usually diagnosed only at surgery or autopsy.
Pulmonary lacerations usually resolve over a period of 3 weeks to a year; although uncommon, they may indefinitely persist as pulmonary nodular opacity; years later, when blood is expectorated, they may appear as pulmonary cysts (Ulutas H, et al. 2015).
More rarely, due to the reduced pulmonary compliance, the laceration is visible as evident gas-filled scarring and extrabronchial development.
Within particularly large lesions, the hematoma may have expanding force and may be associated with hemodynamically significant hemorrhage.
4 Pulmonary Hernia
Lung herniation is an uncommon complication of blunt chest trauma, whereas it is more common with penetrating trauma.
It may occur through either a congenital or an acquired parietal opening, resulting from rib fractures or costochondral or sternoclavicular dislocations.
The anterolateral chest wall is more susceptible to traumatic lung herniation (Fig. 7), because of the minimal muscle thickness (intercostal muscles), compared to the posterior wall, reinforced by strong muscle planes (trapezius, latissimus dorsi, rhomboid).
The intercostal hernias may be associated with a hemothorax or a pneumothorax, secondary to strangulation or incarceration of the lung parenchyma. In symptomatic cases, a rarely necessary surgical reduction is indicated.
5 Atelectasis
Following a blunt chest trauma, large or small parts of the lung parenchyma may present atelectasis, correlated with the following pathogenic mechanisms: obstructive, compressive, passive, and adhesive atelectasis.
The obstructive atelectasis is a consequence of either mucous plugging, foreign bodies (i.e., dentures), endobronchial blood clot, bronchorrhea, or airway rupture. Large lacerated and/or contused areas may cause compressive atelectasis, as a result of passive atelectasis, eliminating contact between the parietal and visceral pleurae, thereby preventing the natural lung expansion.
Finally, the so-called adhesive atelectasis is a condition of primitive alveoli collapse in association with surfactant deficiency, generally caused by concurrent contused phenomena. In the past, atelectasis was associated with dyspnea and fever, but recent studies have not suggested that fever should be considered a sign of some underlying disorder.
5.1 Diagnostic Imaging
Diagnosis of obstructive atelectasis is based on the located reduction of parenchymal volume and air: radiological signs include lobar, segmental, or subsegmental opacity, without the presence of air bronchograms, associated with displacement of fissures, hilum, mediastinum, and ipsilateral hemidiaphragm (Wanek S, Mayberry JC 2004).
In compressive atelectasis, the atelectatic lung becomes visible as radiopaque edge adjacent to the contused/lacerated area. In passive atelectasis, the parenchymal opacity may essentially remain normal, due to the consensual local-regional reduction of air and blood; air bronchogram is frequently visible if bronchial vessels are not filled with secretion or blood, as is the case in adhesive atelectasis.
It must be pointed out that the different types of atelectasis are variously associated in the traumatized. The dense, homogeneous appearance, associated with fissure deviation, allows a differential diagnosis between contusion and pulmonary aspiration.
On MSCT, atelectasis usually demonstrates a greater enhancement after contrast medium, compared to the consolidative lung in contusion, due to the associated crowding of pulmonary vessels. Secondary signs of volume loss are clearly visible, thanks to the MPR reconstructions (Fig. 8).
(a, b) Axial CT scans: wide bilateral atelectasis of lower lobes. The greater enhancement of atelectasis is due to the associated crowding of pulmonary vessels; (c) coronal and (d) sagittal reconstructions clearly demonstrate the pulmonary volume loss. In this patient, associated is an anterobasal bilateral pneumothorax.
References
Cohn SM (1997) Pulmonary contusion: review of the clinical entity. J Trauma 42:973–979
Gaillard M, Hervé C, Mandin L, Raynaud P (1990) Mortality prognostic factors in chest injury. J Trauma 30:93–96
Ianniello S, Di Giacomo V, Sessa B, Miele V (2014) First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. Radiol Med 119: 674–680.
Mayberry JC (2000) Imaging in thoracic trauma: the trauma surgeon’s perspective. J Thorac Imaging 15:76–86
Miele V, Di Giampietro I, Ianniello S, Pinto F, Trinci M (2014) Diagnostic imaging in pediatric polytrauma management. Radiol Med 120:33–49
Peters S, Nicolas V, Heyer CM (2010) Multidetector computed tomography-spectrum of blunt chest wall and lung injuries in polytraumatized patients. Clin Radiol 65:333–338
Rivas LA, Fishman JE, Munera F et al (2003) Multislice CT in thoracic trauma. Radiol Clin North Am 41:599–616
Roy-Choudhury SH, Gallacher DJ, Pilmer J et al (2007) Relative threshold of detection of active arterial bleeding: In vitro comparison of MDCT and digital subtraction angiography. AJR Am J Roentgenol 189:W238–W246
Ryan MF, Hamilton PA, Chu P et al (2004) Active extravasation of arterial contrast agent on post-traumatic abdominal computed tomography. Can Assoc Radiol J 55:160–169
Scaglione M, Pinto A, Pedrosa I et al (2008) Multi-detector row computed tomography and blunt chest trauma. Eur J Radiol 65:377–388
Scott MF, Khodaverdian RA, Shaheen JL et al (2015) Predictors of retained hemothorax after trauma and impact on patient outcomes. Eur J Trauma Emerg Surg. Epub ahead of print
Shanmuganathan K, Mirvis SE (1999) Imaging diagnosis of nonaortic thoracic injury. Radiol Clin North Am 37:533–551
Sivit CJ, Peclet MH, Taylor GA (1989) Life-threatening intraperitoneal bleeding: demonstration with CT. Radiology 71:430
Traub M, Stevenson M, McEvoy S et al (2007) The use of chest computed tomography versus chest X-ray in patients with major blunt trauma. Injury 38:43–47
Trindade LM, Lopes LC, Cipriano GF et al (2009) Alveolar recruitment in pulmonary contusion: case report and literature review. Rev Bras Ter Intens 21:104–108
Ulutas H, Celik MR, Ozgel M et al (2015) Pulmonary pseudocyst secondary to blunt or penetrating chest trauma: clinical course and diagnostic issues. Eur J Trauma Emerg Surg 41:181–188
Van Hise ML, Primack SL, Israel RS et al (1998) CT in blunt chest trauma: indications and limitations. Radiographics 18:1071–1084
Wagner RB, Crawford WO Jr, Schimpf PP (1988) Classification of parenchymal injuries of the lung. Radiology 167:77–82
Wanek S, Mayberry JC (2004) Blunt thoracic trauma: flail chest, pulmonary contusion, and blast injury. Crit Care Clin 20:71–81
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Miele, V., Buquicchio, G.L., Piccolo, C.L., Stasolla, A., Galluzzo, M. (2016). Lung Injury. In: Scaglione, M., Linsenmaier, U., Schueller, G., Berger, F., Wirth, S. (eds) Emergency Radiology of the Chest and Cardiovascular System. Medical Radiology(). Springer, Cham. https://doi.org/10.1007/174_2016_51
Download citation
DOI: https://doi.org/10.1007/174_2016_51
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42582-5
Online ISBN: 978-3-319-42584-9
eBook Packages: MedicineMedicine (R0)