Abstract
Blunt or penetrating trauma to the chest can cause injury to the aorta and its major branching arteries. These injuries are still the second most lethal condition in blunt trauma patients, after head injuries, and need urgent detection and treatment. In this chapter, we will specifically discuss aortic and proximal branch vessel injuries resulting from blunt trauma mechanisms. These are almost invariably resulting from high-impact trauma, usually with rapid deceleration forces. Patients sustaining blunt traumatic aortic injury (BTAI) usually have many concomitant injuries, that will distract from scrutinizing the aorta. This chapter will help radiologist understand BTAI and be a valuable partner in the resuscitation team, both in diagnosis and treatment of BTAI.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Blunt or penetrating trauma to the chest can cause injury to the aorta and its major branching arteries. These potentially life-threatening conditions need urgent detection and treatment. In this chapter, we will specifically discuss aortic and major vessel injuries resulting from blunt trauma mechanisms. Thousands of peer-reviewed scientific publications are available, indicating the interest and debate on a very dynamic topic. Many terms are used in literature to indicate traumatic injury to the aorta, including but not limited to: blunt aortic injury (BAI), traumatic thoracic aortic injury (TTAI), acute traumatic aortic injury (ATAI), acute thoracic aortic trauma (ATAT), traumatic aortic rupture (TAR) and blunt traumatic aortic rupture (BTAR). We elect to use blunt traumatic aortic injury (BTAI), since it indicates blunt trauma as the mechanism and encompasses all injuries within the spectrum. We will give an overview of important issues and our experience with BTAI.
Blunt traumatic injury to the aorta and/or major branching vessels almost invariably results from high-impact trauma, usually with rapid deceleration forces, further detailed in the next section on mechanisms of injury. A well-documented study by Parmley et al. in 1958 demonstrated that around 85 % of victims sustaining BTAI die on the scene or shortly thereafter (Parmley et al. 1958). Improvements in vehicle safety profiles, prehospital care and rapid diagnosis may have improved survival rates. However, this cannot definitively be concluded from the literature over the past six decades. In a study on 881 blunt traumatic fatalities performed in Los Angeles, USA, in 2005, in 304 victims undergoing full autopsy, BTAI was present in 104 (34 %) (Teixeira et al. 2011). Unfortunately, this study does not state the total number of polytrauma patients to give the incidence of BTAI in a population including victims deceased on scene.
A fairly recent large study performed on data collected in the National Trauma Databank in the USA from 2000 to 2005 does have relevant figures on trauma victims transported to hospitals (thus excluding death on scene) (Arthurs et al. 2009). In this study, 3.114 out of 1.1 million trauma patients had BTAI, resulting in an incidence of BTAI in patients alive on scene of 0.3 %. In keeping with literature, the mean age was 41 (±20) and 72 % were males, and the mean injury severity score was 40 (±17). Of this cohort, 113 (4 %) died during transportation to and 599 (19 %) died during triage in the hospital. Of the 2.402 patients surviving transportation and triage, 31 % had major concomitant head injury and 29 % had major abdominal injury (Arthurs et al. 2009).
A meta-analysis with a total of 7258 patients from 90 articles found the following rates of concomitant injuries: orthopaedic fractures in 70 %, thoracic injury in ~50 %, abdominal injury in 40 % and head injury in 37 % (Antonopoulos et al. 2014). In the study by Arthurs et al., two-thirds of patients could not undergo attempts to repair the injury, mostly due to other injuries, and BTAI was found to be an independent prognosticator for poor outcome (Arthurs et al. 2009). The figures in this large study are in keeping with literature in the fact that BTAI despite its relative rarity is still second only to head injury as a cause of death in polytrauma patients. Even compared to matched cohorts with comparable concomitant injuries, BTAI increases risk of mortality fourfold, overall mortality being 55 % (Arthurs et al. 2009).
In patients reaching the hospital with BTAI that can actually receive treatment for their aortic injury, survival rates thereafter are high, in somewhat dated reports form 2008 being estimated in the range of 70–90 % (Steenburg et al. 2008; Demetriades et al. 2008). Further improvement may have occurred since, although, given the concomitant injuries, it is unlikely that survival will ever be close to 100 %. Recent decades have seen important changes in treatment of BTAI, which we will address in a later section. Part of these changes have to do with much more sensitive imaging modalities and more aggressive imaging strategies after trauma, depicting aortic injuries that in more remote decades would not have been picked up.
Despite the fact that patients may survive, associated morbidity will influence most patients’ lives after the traumatic incident. Fully independent feeding will be achieved by 72 %, locomotion by 33 % and expression by 80 %, lower numbers than in cohorts matched for other injuries (Arthurs et al. 2009). This is another indication of the severity of trauma and its impact on life after such an injury.
2 Mechanism of Injury
Since Parmley et al. first published a large cohort of patients in 1958, studies have consistently shown BTAI to be the result of high-impact trauma. Motor vehicle accidents (MVAs), motorcycle and airplane crashes, pedestrians struck by vehicles and falls from height make up the vast majority of cases (Parmley et al. 1958; Teixeira et al. 2011; Antonopoulos et al. 2014; Challoumas and Dimitrakakis 2015; Lin et al. 2016; Fabian et al. 1997; Burkhart et al. 2001).
Injury to the aortic wall is likely a result of any or a combination of the following potential mechanisms, as described by Parmley et al. and others (Parmley et al. 1958; Burkhart et al. 2001; Mosquera et al. 2013; Crass et al. 1990; Cohen et al. 1992; Lundevall 1964; Baqué et al. 2006) (Fig. 1). Direct compression or the so-called osseous pinch may result from the aorta being pinched between the vertebrae and the anterior thoracic skeleton (sternum, clavicles and ribs) (Crass et al. 1990, 1992). Direct penetration from fractured ribs, sternum or vertebrae may also occur. Other mechanisms have their effect in a more indirect manner. Stretching of the aorta from displacement of vertebrae may cause aortic wall injury more remote to the osseous injury site, the so-called ‘stretch’ injury. Extreme pressure in the aortic lumen by compression on the abdomen or lower chest may also cause injury, a mechanism known as the ‘water-hammer’ effect. The water-hammer effect, proposed by Lundevall, results when the flow of a noncompressible fluid is occluded dramatically, which leads to high-pressure waves being reflected back along the vessel wall (Lundevall 1964). At the aortic root, the ligamentum arteriosum attachment and the diaphragmatic crus, the aorta is connected to other tissues, increasing regional strain by different deceleration characteristics of the joined tissues. The final mechanism potentially contributing to injury is torsion, which indicates rotational forces of the aorta along its longitudinal axis. A theory about elevated aortic pressure due to compression of the left ventricle that was proposed in the first decades of the twentieth century has since been dismissed by other scientists (Baqué et al. 2006).
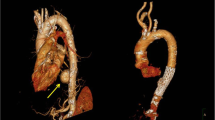
Depending on the forces in play, the aorta injury site can be the root, ascending aorta, arch, isthmus, descending aorta or even abdominal aorta (less common). Multiple studies in deceased and surviving patients show the aortic isthmus is the most common location of injury. However, since studies are not inclusive of all blunt trauma-related fatalities, there may be a shift in numbers with more injuries potentially occurring at the aortic root. A considerable number of patients has aortic injury at multiple sites, in the autopsy series by Teixeira et al. amounting up to 18 % (Teixeira et al. 2011) (Fig. 2). In that study, 2 % of injuries were located at the aortic root, 3 % at the ascending aorta and 11 % at the arch. Mention is warranted for the other upper thoracic major vessels, especially the aortic arch branches, which can be injured in isolation. In a small sample study by Chen et al., 38 % of injuries involved the proximal aortic arch branching vessels (Chen et al. 2001). Even though the percentage likely is lower, injury to these vessels is important to diagnose and treat if necessary.
Example of multilevel blunt traumatic aortic injury on sagittal CTA (a) with corresponding axial CTA slides (b, c). The proximal intimal injury (solid white arrow) was most likely caused by a stretch mechanism; the distal intimal flap (open white arrow) may have been caused by stretch and/or direct impact from the nearby vertebral fracture (arrow head)
3 Terminology and Clinical Issues
The diagnostic and treatment process in polytrauma patients usually takes place in multidisciplinary teams with members of varying level of experience. In combination with stress because of time concerns and multitude of injuries, clear communication is paramount. Therefore, the most important point to make about terminology is that all members of the resuscitation team, including radiology staff, should align the vocabulary used throughout the institution. This also includes which of the many classification schemes is used to grade the injury.
As described in the introduction, many different terms are used in literature to indicate traumatic injury to the aorta after blunt trauma. Further confusion may arise with other terminologies in this setting. Specific terms to be aware of with regard to diagnosis and treatment are mediastinal haematoma, peri-aortic haematoma, minimal aortic injury, pseudo-aneurysm and secondary signs of injury (SSI). We will describe these terms here to minimize confusion.
Mediastinal haematoma is used to describe haematoma within the mediastinum with a fat plane preserved around the aortic adventitia. These haematomas are not considered to be associated to aortic injury, but originate from other sources of bleeding, like mediastinal veins or fractures of vertebrae or sternum (Forman et al. 2013; Raptis et al. 2015) (Fig. 3).
Peri-aortic haematoma is used to describe haematoma directly bordering the aortic adventitia (i.e. loss of peri-aortic fat plane) and either confined to the direct peri-aortic region or extending beyond into the mediastinum (Fig. 4). Although previously reported to occur as a false-positive indirect sign of aortic injury (Steenburg and Ravenel 2008), advances in modern CT techniques pick up previously undetected small injuries. If peri-aortic haematoma is present, the aorta should be scrutinized for presence of injury. If peri-aortic haematoma is absent, this nearly excludes higher-grade aortic injury. However, lesser grade injury is still possible if peri-aortic haematoma is absent, around 21–22 % of such cases occurring without surrounding haematoma (Forman et al. 2013; Aladham et al. 2010).
Minimal aortic injury (MAI, also known as minor aortic injury) is a term used to describe a lesser grade of aortic injury that may resolve with conservative measures, including monitoring, blood pressure control and repeat CT. However, multiple groups that publish on the topic define the term differently. The definition ranges from injuries in which outer aortic wall contour is preserved to those including pseudo-aneurysms of up to 50 % of the normal aorta diameter (Forman et al. 2013; Caffarelli et al. 2010; Rabin et al. 2014a).
Pseudo-aneurysm relates to an aortic injury in which there is (near) complete loss of aortic wall integrity resulting in a regular or an irregular deformity of the outer wall of the aorta (Fig. 5). Especially if there is surrounding haematoma with mass effect on the mediastinum, there is a high chance of rupture (Rabin et al. 2014a, b).
Secondary signs of injury (SSI) were recently defined in a study that sought parameters for successful nonoperative management of BTAI as pseudo-coarctation, extensive mediastinal haematoma (with mass effect) and large left haemothorax (Rabin et al. 2014a, b) (Fig. 6). They concluded that grade 3 aortic injuries (pseudo-aneurysms involving more than 50 % the circumference of the aorta in their study) with SSI needed urgent repair, whereas those without SSI could undergo delayed repair (Rabin et al. 2014a). The use of SSI therefore seems to aid management decisions.
3.1 Classification of BTAI
To grade blunt traumatic aortic injury, several classification systems have been published, the first of which was by Parmley et al. in 1958 on the basis of a large autopsy study (Parmley et al. 1958). Gavant et al. published the first classification system based on CT images in 1999, very comprehensive but somewhat difficult to use (Gavant and Helical 1999). In 17 years since, six more groups published classification systems with different degree of variation, namely, Simeone et al. (2006), Azizzadeh et al. (2009), Caffarelli et al. (2010), Lamarche et al. (2012), Starnes et al. (2012) and Rabin et al. (2014a). The multitude of different classification systems likely reflects local experiences with treatment choices, as well as the rapid improvement of CT technology and endovascular stent grafts used for treatment. In 2011, the Society for Vascular Surgery published clinical practice guidelines for endovascular repair of BTAI (Lee et al. 2011), using the classification system by Azizzadeh et al. (2009). However, this was before other classification systems were published. The Vancouver Simplified classification system in the study by Lamarche et al. found better interobserver agreement than the Simeone and Gavant classifications, the reason for which we like to use it (Lamarche et al. 2012). As mentioned before, the most important issue for all team members involved in caring for BTAI patients remains to make sure to use the same terminology and classification.
The Vancouver classification, like most other classifications, has four grades (Fig. 7). Grade 1 and grade 2 essentially have preserved outer aortic contours and consist of luminal thrombus, intimal flap and/or intramural haematoma, these lesions in grade 1 being smaller than 1 cm and in grade 2 larger than 1 cm. Grade 3 and grade 4 lesions demonstrate abnormality of the outer wall of the aorta, with grade 3 lesions being pseudo-aneurysms of any size and grade 4 lesions showing frank contrast extravasation. Given the fact that some publications show good results of conservative management as treatment for smaller pseudo-aneurysms, caregivers may elect to use other classification systems.
Vancouver classification of blunt traumatic aortic injury. Grade 1 injuries (luminal thrombus, intimal flap or intramural haematoma) are less than 1 cm; if larger than 1 cm, injuries are grade 2; aortic pseudo-aneurysms are grade 3; and grade 4 are injuries with active contrast extravasation indicating ongoing haemorrhage (From Lamarche et al. (2012), Reply to the Editor, copyright 2012. Reprinted with permission from Elsevier)
3.2 Clinical Issues
Clinical symptoms and signs are non-specific for BTAI, nor sensitive. Patients may have chest pain, back pain or difficulty breathing, and signs include external chest wall injuries, systemic hypotension, concomitant upper limb hypertension with lower limb hypotension or a substantial difference in blood pressures between the right and left brachial arteries (present in up to 50 % of patients with BTAI). Some patients may present initially with no clinical signs but rapidly develop hemodynamic instability (Steenburg et al. 2008; Raptis et al. 2015). Factors negatively influencing prognosis are a systolic blood pressure <90 mmHg and hypothermia with T < 35 °C and injury severity score (ISS) >25 (Arthurs et al. 2009).
As stated before, blunt traumatic aortic injury invariably is the result of high-energy trauma to the chest and most often is not confined to this anatomic area. In most cases, significant concomitant injuries are present. Depending on the severity of the aortic injury, the hemodynamic stability of the patient and the severity of the other injuries, treatment priorities have to be decided. If possible, repair of BTAI should be delayed for favourable outcome, especially in concomitant head injuries (Fox et al. 2015; Rabin et al. 2014b). This will also increase the time to carefully evaluate the extent of other injuries. If aortic injury and traumatic brain injury coexist, research has shown that the most unstable injury should be prioritized to immediate care. It also suggests that intracranial haemorrhage is not a contraindication to endovascular aortic stenting or an absolute contraindication to systemic anticoagulation during this procedure (Fox et al. 2015; Kitagawa et al. 2013).
To predict which patients need urgent repair instead of delayed repair, Harris et al. proposed a new aortic injury score to predict early rupture (Harris et al. 2015). From their study, they conclude that a patient is at high risk of early rupture if any two of the following three factors are present: lactate >4 mM, posterior peri-aortic haematoma >10 mm or lesion/normal aortic ratio >1.4 (meaning an aortic diameter more than 40 % increased compared to the nearest normal aortic diameter). Whether these criteria are better predictors of the need of urgent repair of grade 3 injuries than the secondary signs of injury (SSI) defined by Rabin et al. (2014a, b) (see before) remains to be seen. Likely, the criteria of both study groups overlap, but these findings will help select patients that need urgent instead of delayed treatment.
4 Imaging
Post-intravenous contrast CT angiography (CTA) is the standard diagnostic test for detection of thoracic aortic and branch vessel injury (Fox et al. 2015). The sensitivity is 96 %, specificity is 100 % and negative predictive value 99.9 %. These percentages are by far superior when compared to plain chest radiography, transoesophageal echography (TEE) or conventional arch aortography (Steenburg and Ravenel 2008). Furthermore, CTA is very accurate in detection of most other chest injuries, which exist with or without the presence of BTAI. However, other imaging modalities can be useful, so we will discuss strengths, weaknesses and findings of those as well.
4.1 Radiography
Although CT is increasingly being used as the primary imaging modality in trauma resuscitation, chest radiography (CXR) in many centres is still used as the first adjunct to the primary survey. Signs seen on plain films are either sensitive or specific, but never both; therefore, utility of CXR in the setting of suspected BTAI is low (Nagy et al. 2000; Cook et al. 2001; Gutierrez et al. 2016). Especially in the case of MAI, modern CTA can demonstrate BTAI without changes to the outer wall of the aorta and even without bordering haematoma, further underscoring the potential to miss these injuries on CXR. However, signs can still be present on a conventional chest X-ray and, if so, prompt for further evaluation with CTA (Fig. 8).
A 27-year-old woman struck by a car while on moped. Supine AP chest X-ray taken during resuscitation with unsuspected findings consistent with aortic injury (a): indistinct aortic contour (white solid arrows), depressed left main bronchus (open black arrow) and apical cap consistent with haemorrhage extending to the pleural space (solid black arrows). Injury was proven with CT (b): aortic arch (open white arrow) demonstrates frank extravasation (solid white arrows) into the pleural cavity (white asterisks), consistent with grade 4 injury. Note the homogenous low density of the haemothorax, indicating hyperacute exsanguination with lack of time to form cloth. Patient did not survive to treatment
Signs in decreasing order of sensitivity according to Cook et al. are as follows: mediastinal width >8 cm (sens 90 %, spec 30 %), mediastinum-to-chest width ratio >0.25 (sens 90 %, spec 6 %), opacified AP window (sens 90 %, spec 51 %), irregular aortic knob (sens 80 %, spec 68 %), blurred aortic contour (sens 70 %, spec 53 %), nasogastric tube deviation (sens 50 %, spec 91 %) and trachea shifted to patient’s right (sens 40 %, spec 86 %) (Cook et al. 2001).
Signs in decreasing order of specificity are as follows: thoracic spine fracture (spec 93 %, sens 11 %), first rib fracture (spec 91 %, sens 10 %), NG tube deviation (spec 91 %, sens 50 %), depressed left main bronchus (spec 90 %, sens 10 %), wide left paraspinal line (spec 90 %, sens 29 %), clavicle fracture (spec 87 %, sens 0 %), trachea shift to patient’s right (spec 86 %, sens 40 %), left apical cap (spec 80 %, sens 20 %) and pulmonary contusion (spec 72 %, sens 30 %) (Cook et al. 2001).
Rather than spending a lot of time analysing all separate findings and measurements, a general assessment of the mediastinum and decision to ‘normal’ or ‘abnormal’ results in better sensitivity and interobserver agreement (Ho et al. 2002). If the only abnormality seen on an initial screening supine anteroposterior CXR is mediastinal width more than 8 cm, it can be worthwhile repeating the CXR standing and posteroanterior, in which case, 38 % of exams will be normal (Schwab et al. 1984). However, we fully agree with Raptis et al. and others that patients with an abnormal CXR, patients with high index of suspicion for BTAI or patients with chest pain out of proportion to their known injuries after appropriate trauma need to proceed to CTA of the chest (Raptis et al. 2015; Fox et al. 2015).
4.2 Angiography/Aortography
The publication of the Eastern Association for the Surgery of Trauma (EAST) practice management guideline for the diagnosis and management of blunt aortic injury in 2000 still defined angiography as the ‘gold standard’ for the diagnosis of BTAI. However, the workgroup already acknowledged that ‘CT scanning is taking more of a role, especially for screening’ (Nagy et al. 2000). Since their publication, rapid developments of CT techniques have rendered CTA more sensitive than conventional angiography, mostly due to the detection of extra-luminal abnormalities, either confined to the aortic wall or beyond. This has caused the same society to revise their guidelines, which in their publication in 2015 strongly recommend CT with intravenous contrast for the diagnosis of BTAI (Fox et al. 2015). Angiography is of course still used if endovascular treatment for BTAI is undertaken (Fig. 9).
4.3 Abdominal and Transthoracic Ultrasound
During trauma resuscitation, many centres will include an ultrasound scan according to the focussed abdominal sonography in trauma (FAST) as an adjunct to the primary survey. A FAST examination essentially is a quickly performed ultrasound to demonstrate the presence or absence of free intraperitoneal fluid by evaluating the four abdominal quadrants. In addition, one can look for presence of pericardial effusion, pleural effusion and/or pneumothorax in a reasonably quick and reliable fashion, the so-called extended FAST (e-FAST). Although e-FAST could demonstrate a secondary sign of injury in BTAI, notably large left haemothorax, or demonstrate pericardial effusion, the aorta itself usually is poorly visualized and can only be examined below the diaphragm. The same holds true for transthoracic ultrasound.
4.4 Transesophageal Echocardiography (TOE or TEE)
Already in 2008, Demetriades et al. found that between 1997 and 2007, there had been a near elimination of transoesophageal echocardiography for the diagnosis of BTAI, dropping from nearly 12 % of BTAI patients receiving TOE in 1997 to 1 % in 2007 (Demetriades et al. 2008). The primary use currently is to evaluate cardiac dysfunction and injury or hemodynamic state and response to treatment. TOE can be used to evaluate the descending aorta, being reasonably sensitive for traumatic aortic injury in that location but overall only moderately sensitive (Patel et al. 2003; Rippey and Royse 2009). In hemodynamically unstable patients, transoesophageal echocardiography can be used as bedside test, and the probe can remain in place even in the operating theatre.
4.5 Intravascular Ultrasound (IVUS)
In two papers by Williams et al. in the early 1990s, the use of IVUS is discussed as a tool to be used in equivocal angiographic results for BTAI (Williams et al. 1992; Williams et al. 1993). The limitation of this technique as an initial diagnostic test due to practical restrains was already discussed in their second paper and has not been altered since. Malhotra et al. as well as Patel et al. demonstrated better sensitivity compared to angiography especially for picking up MAI, before the era of CTA as a gold standard (Patel et al. 2003; Malhotra et al. 2001). A more recent paper again proved IVUS to be better than angiography in patients where CTA findings were equivocal. Therefore, the authors advocated the use of IVUS in potential TAI patients in whom angiography is being considered (Azizzadeh et al. 2011). However, the nature of the procedure requires vascular access, with another option to rule out aortic injury being a repeat CTA, with or without ECG triggering. If a patient is managed with endovascular stent-graft placement, IVUS has been shown to be useful for selection of stent-graft size (Wallace et al. 2015; Shi et al. 2015). Compared to the acute CTA, IVUS during the procedure of stent placement demonstrates a larger aortic diameter, possibly reflecting intravascular hypovolemia during resuscitation at initial imaging, necessitating preoperative reassessment of aortic lumen diameter (Wallace et al. 2015).
4.6 Magnetic Resonance Imaging (MRI)
Length of examination time, limited accessibility, non-compliant materials and relatively small bore sizes render MRI unfeasible in the initial assessment of patients with multiple injuries. In patients with equivocal CTA findings for BTAI, an MRI study can be considered if they are hemodynamically stable and also otherwise able to undergo the examination. Fattori et al. published two papers in the mid- to late 1990s on the use of MRI for the diagnosis of acute BTAI and for follow-up in the delay to treatment, demonstrating its feasibility (Fattori et al. 1996; Fattori et al. 1998). The paucity of results when performing literature searches to find the use of MRI in BTAI indicates the limited role for this modality especially in the acute phase, despite the well-documented use in other aortic and major vessel diseases.
4.7 Computed Tomography Angiography (CTA)
As stated before, CTA now is the gold standard for the evaluation of BTAI, given its high accuracy and near-perfect negative predictive value. In these usually severely injured polytrauma patients, the chest will oftentimes be imaged in conjunction with the abdomen and pelvis.
4.8 CT Technique
Different protocols exist to administer iodinated intravenous (IV) contrast material, with either single-bolus, split-bolus or triple-bolus administration being used. To avoid streak artefacts from high concentrations of iodine in the left brachiocephalic vein, IV contrast material should preferably be administered via the right arm whenever possible. Depending on scanner manufacturer and type, an empirically fixed delay or a bolus-triggering mode can be used. The administration of a separate timing bolus before the definitive scan is not commonly chosen in current practice, mostly due to time constrains. Furthermore, with current technical advances in multi-detector computed tomography (MDCT) resulting in high spatial resolution, vascular injuries will be detected even if acquisition phase is past proper arterial phase, which still is the preferred phase of acquisition (Raptis et al. 2015). In our opinion, the radiologist should be present at the acquisition to decide if image quality is satisfactory and to instantaneously order repeat scan or extra phases, especially for the abdomen and pelvis.
When evaluating the aorta, care should be taken to adjust window and level settings as to not mask minimal luminal or mural abnormalities. Specific Hounsfield unit (HU) settings are difficult to give, since the correct window/level setting varies with attenuation values in each scan (depending on kVp, iodine concentration and flow rate of IV contrast administered). In some institutions, a non-contrast scan is obtained prior to the scan with IV contrast to rule out intramural haematoma (IMH), which in our experience is not as important as with aortic dissection protocols. If during the evaluation at the scanner console there is doubt about the presence of IMH, a late-phase CT after 10–15 min can be obtained to evaluate for increased aortic wall attenuation; this however is rarely needed. If uncertainty of aortic injury is caused by artefacts, a repeat scan can be obtained, applying ECG triggering if caused by cardiac pulsation (Fig. 10). Positioning of external lines and arms may further alter image quality.
Initial routine CTA without ECG triggering (a, b) and follow-up ECG-triggered CTA (c, d). Small, <1 cm intimal flap with thrombus is identified in the ascending aorta just distal to the origin of the left coronary artery (arrows). Although this clinically significant finding was suspected on the initial CTA without ECG triggering, it is appreciated far superiorly on the ECG-triggered CTA
It is paramount to use thin slices of the original axial dataset for evaluation, and multiplanar reformations (MPRs) should be made, preferably interactively at a workstation or similar server-based software or by MPRs made by technicians according to preset protocols. A sagittal-oblique reconstruction, also referred to as ‘candy stick’ reconstruction, is especially useful since it shows the entire length of the thoracic (and possibly abdominal) aorta (Fig. 11). Interventional radiologists and surgeons will like the view for the fact that it resembles the oblique view obtained when performing angiography.
4.9 Imaging Findings
Since CT in nearly all cases will be the chosen modality to detect BTAI, we will describe the features of aortic injury here. However, findings on other imaging modalities will be very similar to those seen on CT. After blunt trauma, CT signs of aortic injury can be located at any section of the aorta and can even be present at multiple sites, especially after stretch mechanisms. The most common location to find BTAI on imaging is the aortic isthmus. Signs can be divided in direct and indirect signs of BTAI.
Direct signs are very sensitive and specific for BTAI; however, false positives and false negatives do occur, either caused by technical issues (artefacts) or misinterpretation. Direct signs demonstrate aortic wall changes and make up the grades of aortic injury, irrespective of which classification system is used. Luminal thrombus abutting the intima, an intimal flap and intramural haematoma (IMH) can be seen and depending on size smaller or larger than 1 cm will be grade 1 or grade 2 injuries, respectively (Vancouver classification) (Lamarche et al. 2012). Luminal thrombus abutting the intima oftentimes is demonstrated as a small, round contrast-filling defect on the axial images; however, it can have a more oblong configuration, especially on MPRs (Fig. 12). An intimal flap is a more linear hypodense structure projecting into the lumen of the aorta, connected to the wall (Fig. 13). One very specific and more severe form of intimal flap is circumferential dehiscence of the intima, creating intimo-intimal intussusception, which is demonstrated by a more or less regular circular and linear hypodense line within the aortic lumen (Fig. 14). IMH can be seen as thickening of the aortic wall, separating the intima and adventitia by haematoma in the media. IMHs can be focal or rather long and usually are not circumferential (Fig. 15). If a non-contrast enhanced CT is performed, this portion of the aortic wall will demonstrate increased attenuation (around 40–60 HU), a feature that is less obvious if contrast was given. However, in our experience, the non-contrast scan is not needed to make a confident diagnosis of IMH, given modern-day MDCT resolution.
Grade 3 injuries demonstrate outward contour deviations of the aorta, so-called pseudo-aneurysms, that can be relatively regular or irregular, the latter likely being more unstable than the former (Figs. 4 and 5). If pseudo-aneurysms are small, they can be difficult to pick up given the orientation in a curved plane in three dimensions, rendering the use of MPRs even more important (Fig. 16). In grade 4 injuries, active extravasation of IV contrast is seen, either from an otherwise fairly normal aorta, or at the site of a (usually irregular) pseudo-aneurysm (Figs. 8 and 17) Needless to say, this is an indication for urgent repair, either by endovascular stent graft or open thoracotomy procedure.
Axial (a) and coronal (b) CTA showing traumatic aortic rupture at the level of the arch with active contrast extravasation (arrow, same patient as Fig. 8). Large mediastinal haematoma and large left-sided haemothorax. Patient deceased prior to treatment
Indirect signs of aortic injury mostly relate to the bleeding from the aortic injury in the immediate peri-aortic region or beyond. Peri-aortic haematoma, as described before, is haematoma that abuts the aortic adventitia and obliterates the peri-aortic fat plane (Fig. 4) Larger haematomas will extend further into the mediastinum and are slightly hyperdense (40–70 HU). Bleeding from the aortic injury can extend into the pleural space or pericardium, depending on the location of the injury, giving rise to haemothorax or haemopericardium. Usually haemopericardium is homogenously hyperdense, whereas haemothorax can have mixed densities with more hyperdense areas indicating cloth (Fig. 6). However, if pleural effusion has densities similar to fluid (0–20/30 HU), it can be difficult to differentiate hyperacute haematoma from reactive effusion (Fig. 8).
Two indirect signs can be seen on abdominal CT and should mandate further investigation of the thoracic aorta. These are obliteration of the retro-crural peri-aortic fat (possibly indicating caudal extension of more cranially located peri-aortic haematoma) (Fig. 18) and otherwise unexplained acute renal infracts, especially if bilateral, that can originate from luminal thrombus of more cranially located BTAI.
5 Differential Diagnosis and Pitfalls
In the setting of sustained high-energy trauma, a high index of suspicion for BTAI is warranted. Differential diagnoses that can be mistaken for BTAI mainly reside around the level of the isthmus, namely, a ductus diverticulum, patent ductus arteriosus and aortic spindle. Confusion may also arise more proximally from the nearby superior intercostal vein if opacified by contrast and in younger patients from remaining thymic tissue. Knowing normal anatomy will help discerning these entities from BTAI. A ductus diverticulum is located at the aortic attachment of the ligamentum arteriosum, the former entry to the ductus arteriosus. In contrast with BTAI, a ductus diverticulum has smooth, obtuse angles with the aortic wall, whereas BTAI usually is more irregular and steeply angled and oftentimes has abutting peri-aortic haematoma (Fig. 19) A patent ductus arteriosus is a rarity in itself and therefore a fairly remote option as a differential diagnosis. It can be recognized as a tubular structure with regular contours, where the differential of active contrast extravasation in BTAI usually is irregular and situated within haematoma. Aortic spindles are located just distal to the isthmus and are smooth, regular fusiform mild dilatations of the aorta, again without peri-aortic haematoma (Fig. 19).
Issues related to imaging technique may also cause difficulty in image interpretation, pitfalls mostly being related to artefacts caused by motion and pulsation or due to beam hardening (if the acquisition was performed with arms down). As mentioned before, if IV contrast was administered via the left arm, high concentration of iodine in the left brachiocephalic vein may cause streak artefacts that can hamper assessment of especially the proximal branching vessels. Artefacts can oftentimes be distinguished by evaluation of other structures, such as other vessels or the skin. However, if artefacts are a major concern, a repeat examination with arms up and ECG triggering where possible should be obtained (Fig. 10).
6 Delayed Presentation Injuries
Blunt traumatic injuries to the thoracic aorta and its branch vessels are rare and seldom occur as the sole traumatic entity (Antonopoulos et al. 2014). As mentioned before, patients usually suffer many concomitant injuries and will almost always undergo whole-body MDCT. This modality has an extremely high negative predictive value for blunt traumatic aortic injuries. Although incidence of delayed presentation injuries is unknown, false-negative studies can occur, with missed thoracic aortic injuries following their natural course. Pseudo-aneurysms can be detected incidentally after remote trauma, or they can cause clinical symptoms due to mass effect on surrounding tissues (Fig. 20) or potentially rupture.
7 Proximal Aortic Branch Vessel Injury
In the late 1990s, research demonstrated injuries to the major thoracic branches of the aorta in a considerable number of patients, either with presence of aortic injury, or in isolation. In a well-documented study by Ahrar et al. in 89 patients undergoing angiography for expected BTAI, 17 patients (19 %) had 24 injuries to the aortic arch branches. In 14 of these 17 patients, the aorta was intact, whereas three patients also had aortic rupture, resulting in 16 % of patients having isolated branch vessel injury (Ahrar et al. 1997). The study by Chen et al. revealed aortic branch vessel injuries in one-third of patients who sustained vascular injury from blunt trauma and underwent aortography (Chen et al. 2001). Despite these figures, proximal brachiocephalic arterial injuries due to blunt trauma remain quite rare (Galan et al. 1992; LoCicero and Mattox 1989; Prêtre and Chilcott 1997; Shorr et al. 1987). The innominate artery accounts for 50 % of these injuries and is the second most common injured vessel after the thoracic aorta (Prêtre et al. 1997). The left common carotid and left subclavian artery account for the remaining injuries.
Vessel injuries of the innominate and left common carotid artery tend to occur proximal at the vessel origin (Rosenberg et al. 1989; Karmy-Jones et al. 2003; Symbas et al. 2005). Anatomically this is where the vessel is tightly fixed onto the aortic arch, whereas the distal part is more mobile and flexible.
In contrast, blunt subclavian artery injuries are located more distally (Costa and Robbs 1988; Cox et al. 1999). These can be explained by adding the direct force of posterior dislocated clavicles. This mechanism might also explain proximal right common carotid artery injury (Fig. 21).
Axial (a) and coronal CTA (b) depict a traumatic pseudo-aneurysm of the proximal right common carotid artery (white arrows). Mechanism of injury was a posterior dislocation of the medial right clavicle. The pseudo-aneurysm was successfully treated with a covered stent; procedural angiograms show stent placement (c–e) to exclude the pseudo-aneurysm (black arrows)
Given its proximity to the aortic arch, most injuries are treated surgically, either by primary repair or prosthetic graft interposition. Endovascular management however should always be considered, whether being definite or as a bridge to surgery (Shalhub et al. 2011).
Venous injuries are rarely encountered in isolation after blunt traumatic injuries to the chest.
8 Management and Treatment for BTAI
In the era of arch aortography as the gold standard for diagnosing traumatic injury to the thoracic aorta and its branch vessels, detected injuries were managed surgically or by medical treatment. In the late 1990s, thoracic endovascular aortic repair (TEVAR) was added a third treatment option for BTAI (Semba et al. 1997; Kato et al. 1997; Rousseau et al. 1999). Despite a lack of randomized controlled trials, the available literature demonstrates a superiority of TEVAR in aortic injury-related mortality, stroke and spinal cord injury as compared to open surgical repair (Azizzadeh et al. 2013; Takagi et al. 2008; Pang et al. 2015; Tang et al. 2008). In 2011, the Society for Vascular Surgery published clinical practice guidelines for the treatment of BTAI in which a TEVAR first policy is advocated based on those studies (Lee et al. 2011). They supported the already ongoing shift in management from open surgical repair to TEVAR. However, despite promising short-term outcomes, questions remain regarding long-term durability of TEVAR in the often reasonably young polytrauma patient. Therefore, several trauma centres still perform open repair awaiting long-term outcomes.
With modern CT picking up subtle injuries that went undetected before, many surgeons have now adopted a management approach of BTAI tailored to the specific aortic injury. Minimal aortic injury possibly does not require immediate endovascular or open surgical repair (Malhotra et al. 2001). These patients are managed with aggressive blood pressure control with systolic blood pressure <100 mmHg and heart rates of 60–80 bpm. These aortic injuries are closely followed with serial CTA at 24 h, every 48–72 h for 7 days and after 4 weeks (Fig. 22).
46-year-old male involved in MVA. Initial CTA (a, b) demonstrates a small pseudo-aneurysm of the proximal descending aorta (solid white arrows) with peri-aortic haematoma. This was treated conservatively with controlled hypotension and close CTA follow-up. CTA at 1-day follow-up (not shown) revealed no interval change. However, CTA at 7 days follow-up (c, d) showed an increase in size of the pseudo-aneurysm (open white arrows). Patient underwent subsequent TEVAR (e, f)
The vascular injuries that require immediate intervention have been clustered in the term severe aortic injury (SAI). Traditionally these included traumatic aortic pseudo-aneurysms and contrast extravasation on CTA. There is however a wide variety on the definitions of MAI and SAI. Consequently, the management of BTAI varies per operator and amongst trauma centres. Recent research shows that an expectant approach is also justified for patients with small traumatic pseudo-aneurysms, previously considered SAI (Caffarelli et al. 2010; Rabin et al. 2014a).
Once the decision for TEVAR is made, thin-slice CTA with multiplanar and three-dimensional reconstruction allows for appropriate visualization of the vascular injuries and planning for TEVAR (Fig. 11). Diagnostic arch aortography in TEVAR planning is obsolete with modern CTA and only performed as part of the TEVAR procedure. Pre-procedure CT images should be assessed for TEVAR eligibility, with absolute contraindication for TEVAR being anatomic ineligibility, mostly due to luminal diameter issues.
The commercially available, on-stock stent grafts require a minimum and maximum diameter and length of the proximal and distal landing zones of the aorta. The diameters vary per manufacturer, but typically range from around 16–46 mm. Under-sizing can lead to failure of proximal and/or distal seal, leading to a type I endoleak. Oversizing also increases the risk of inappropriate sealing due to infolding of the stent graft. A severe complication of oversizing is stent-graft collapse with acute aortic occlusion. Most manufacturers recommend oversizing by 10–20 %.
The diameter of the aorta is influenced by the hemodynamic status of the patient (Chandra et al. 2012; Jonker et al. 2010). Hemodynamically unstable patients have smaller diameters and require more oversizing than hemodynamically stable patients. Care should be taken that the abdominal aorta, iliac and common femoral arteries are of sufficient diameter to deliver the stent graft. The profile of the delivery systems continues to decrease in size, but a minimum of 6–7 mm is recommended. In case of severe aorto-iliac stenosis or occlusions, an abdominal conduit can be used to deliver the stent graft to the thoracic aorta.
Obtaining sufficient proximal seal can require covering of the left subclavian artery (LSA). In the emergency setting, complex endovascular solutions with branched or fenestrated devices are not possible. Re-vascularising the LSA subsequent to covering by TEVAR has long been subject to debate. For TEVAR of aortic aneurysms and dissections, covering of the LSA without revascularization used to be liberally performed. However, more recent published data on TEVAR for aneurysm and type B aortic dissection repair reveal a favourable stroke rate if revascularization is performed prior to TEVAR (Waterford et al. 2016). The Society of Vascular Surgery advocates routine revascularization in elective TEVAR. In patients who need urgent TEVAR with LSA covering, revascularization should be individualized and addressed expectantly on the basis of anatomy, urgency and availability of surgical experience (Lee et al. 2011).
Follow-up imaging after TEVAR aims to diagnose potential adverse events such as device migration, disconnection or endoleak, which might need additional treatment. These have been reported to occur; however, there are no guidelines regarding follow-up imaging after TEVAR for BTAI. Imaging strategies often consist of serial CTA, commonly before discharge for baseline and then at 1, 6 and 12 months followed by annual control. This strategy induces high radiation exposure in a generally young patient population. Long-term data are needed to identify risk factors for potential adverse affects in order to limit this radiation exposure. If patients received an MRI-compatible stent graft, MRI can be used for follow-up, decreasing radiation dose.
References
Ahrar K, Smith DC, Bansal RC, Razzouk A, Catalano RD (1997) Angiography in blunt thoracic aortic injury. J Trauma Inj Infect Crit Care 42(4):665–669
Aladham F, Sundaram B, Williams DM, Quint LE (2010) Traumatic aortic injury: computerized tomographic findings at presentation and after conservative therapy. J Comput Assist Tomogr 34(3):388–394
Antonopoulos CN, Sfyroeras GS, Kallinis A, Kakisis JD, Liapis CD, Petridou ET (2014) Epidemiology of concomitant injuries in traumatic thoracic aortic rupture: a meta-analysis. Vascular 22(6):395–405
Arthurs ZM, Starnes BW, Sohn VY, Singh N, Martin MJ, Andersen CA (2009) Functional and survival outcomes in traumatic blunt thoracic aortic injuries: an analysis of the National Trauma Databank. J Vasc Surg 49(4):988–994
Azizzadeh A, Keyhani K, Miller CC, Coogan SM, Safi HJ, Estrera AL (2009) Blunt traumatic aortic injury: initial experience with endovascular repair. J Vasc Surg 49(6):1403–1408
Azizzadeh A, Valdes J, Miller CC, Nguyen LL, Estrera AL, Charlton-Ouw K et al (2011) The utility of intravascular ultrasound compared to angiography in the diagnosis of blunt traumatic aortic injury. J Vasc Surg 53(3):608–614
Azizzadeh A, Charlton-Ouw KM, Chen Z, Rahbar MH, Estrera AL, Amer H et al (2013) An outcome analysis of endovascular versus open repair of blunt traumatic aortic injuries. J Vasc Surg 57(1):108–114; discussion 115
Baqué P, Serre T, Cheynel N, Arnoux P-J, Thollon L, Behr M et al (2006) An experimental cadaveric study for a better understanding of blunt traumatic aortic rupture. J Trauma Inj Infect Crit Care 61(3):586–591
Burkhart HM, Gomez GA, Jacobson LE, Pless JE, Broadie TA (2001) Fatal blunt aortic injuries: a review of 242 autopsy cases. J Trauma Inj Infect Crit Care 50(1):113–115
Caffarelli AD, Mallidi HR, Maggio PM, Spain DA, Miller DC, Mitchell RS (2010) Early outcomes of deliberate nonoperative management for blunt thoracic aortic injury in trauma. J Thorac Cardiovasc Surg 140(3):598–605
Challoumas D, Dimitrakakis G (2015) Advances in the treatment of blunt thoracic aortic injuries. Injury 46(8):1431–1439
Chandra V, Greenberg JI, Maggio P, Mell MW, Lee JT (2012) Aortic diameter varies in trauma patients: a function of hemodynamic status. J Vasc Surg Elsevier Inc 56(2):586–587
Chen MY, Regan JD, D'Amore MJ, Routh WD, Meredith JW, Dyer RB (2001) Role of angiography in the detection of aortic branch vessel injury after blunt thoracic trauma. J Trauma Inj Infect Crit Care 51(6):1166–1171; discussion 1172
Cohen AM, Crass JR, Thomas HA, Fisher RG, Jacobs DG (1992) CT evidence for the “osseous pinch” mechanism of traumatic aortic injury. AJR Am J Roentgenol 159(2):271–274
Cook AD, Klein JS, Rogers FB, Osler TM, Shackford SR (2001) Chest radiographs of limited utility in the diagnosis of blunt traumatic aortic laceration. J Trauma Inj Infect Crit Care 50(5):843–847
Costa MC, Robbs JV (1988) Nonpenetrating subclavian artery trauma. J Vasc Surg 8(1):71–75
Cox CS, Allen GS, Fischer RP, Conklin LD, Duke JH, Cocanour CS et al (1999) Blunt versus penetrating subclavian artery injury: presentation, injury pattern, and outcome. J Trauma Inj Infect Crit Care 46(3):445–449
Crass JR, Cohen AM, Motta AO, Tomashefski JF, Wiesen EJ (1990) A proposed new mechanism of traumatic aortic rupture: the osseous pinch. Radiology 176(3):645–649
Demetriades D, Velmahos GC, Scalea TM, Jurkovich GJ, Karmy-Jones R, Teixeira PG et al (2008) Diagnosis and treatment of blunt thoracic aortic injuries: changing perspectives. J Trauma 64(6):1415–1418; discussion 1418–1419
Fabian TC, Richardson JD, Croce MA, Smith JS, Rodman G, Kearney PA et al (1997) Prospective study of blunt aortic injury: multicenter trial of the American Association for the Surgery of Trauma. J Trauma Inj Infect Crit Care 42(3):374–380; discussion 380–383
Fattori R, Celletti F, Bertaccini P, Galli R, Pacini D, Pierangeli A et al (1996) Delayed surgery of traumatic aortic rupture. Role of magnetic resonance imaging. Circulation 94(11):2865–2870
Fattori R, Celletti F, Descovich B, Napoli G, Bertaccini P, Galli R et al (1998) Evolution of post-traumatic aortic aneurysm in the subacute phase: magnetic resonance imaging follow-up as a support of the surgical timing. Eur J Cardiothorac Surg 13(5):582–586; discussion 586–587
Forman MJ, Mirvis SE, Hollander DS (2013) Blunt thoracic aortic injuries: CT characterisation and treatment outcomes of minor injury. Eur Radiol 23(11):2988–2995
Fox N, Schwartz D, Salazar JH, Haut ER, Dahm P, Black JH et al (2015) Evaluation and management of blunt traumatic aortic injury: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 78(1):136–146
Galan G, Peñalver JC, París F, Caffarena JM, Blasco E, Borro JM et al (1992) Blunt chest injuries in 1696 patients. Eur J Cardiothorac Surg 6(6):284–287
Gavant ML, Helical CT (1999) grading of traumatic aortic injuries. Impact on clinical guidelines for medical and surgical management. Radiol Clin North Am 37(3):553–574, vi
Gutierrez A, Inaba K, Siboni S, Effron Z, Haltmeier T, Jaffray P et al (2016) The utility of chest X-ray as a screening tool for blunt thoracic aortic injury. Injury 47(1):32–36
Harris DG, Rabin J, Kufera JA, Taylor BS, Sarkar R, O’Connor JV et al (2015) A new aortic injury score predicts early rupture more accurately than clinical assessment. J Vasc Surg 61(2):332–338
Ho RT, Blackmore CC, Bloch RD, Hoffer EK, Mann FA, Stern EJ et al (2002) Can we rely on mediastinal widening on chest radiography to identify subjects with aortic injury? Emerg Radiol 9(4):183–187
Jonker FH, Verhagen HJ, Mojibian H, Davis KA, Moll FL, Muhs BE (2010) Aortic endograft sizing in trauma patients with hemodynamic instability. J Vasc Surg 52(1):39–44
Karmy-Jones R, DuBose R, King S (2003) Traumatic rupture of the innominate artery. Eur J Cardiothorac Surg 23(5):782–787
Kato N, Dake MD, Miller DC, Semba CP, Mitchell RS, Razavi MK et al (1997) Traumatic thoracic aortic aneurysm: treatment with endovascular stent-grafts. Radiology 205(3):657–662
Kitagawa RS, Van Haren RM, Yokobori S, Cohen D, Beckerman SR, Ahmad F et al (2013) Management of simultaneous traumatic brain injury and aortic injury. J Neurosurg 119(2):324–331
Lamarche Y, Berger FH, Nicolaou S, Bilawich A-M, Louis L, Inacio JR et al (2012) Vancouver simplified grading system with computed tomographic angiography for blunt aortic injury. J Thorac Cardiovasc Surg. 144(2):347–354, 354.e1
Lee WA, Matsumura JS, Mitchell RS, Farber MA, Greenberg RK, Azizzadeh A et al (2011) Endovascular repair of traumatic thoracic aortic injury: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg Elsevier Inc 53(1):187–192
Lin C-C, Liu K-S, Chen H-W, Huang Y-K, Chu J-J, Tsai F-C et al (2016) Blunt aortic injury: risk factors and impact of surgical approaches. Surg Today 46(2):188–196. doi: 10.1007/s00595-015-1152-0. Epub 2015 Apr 7
LoCicero J, Mattox KL (1989) Epidemiology of chest trauma. Surg Clin North Am 69(1):15–19
Lundevall J (1964) Traumatic rupture of aorta-with special reference to road accidents. Acta Pathol Microbiol Scand Acta pathologica et microbiologica Scandinavica 62:29–33
Malhotra AK, Fabian TC, Croce MA, Weiman DS, Gavant ML, Pate JW (2001) Minimal aortic injury: a lesion associated with advancing diagnostic techniques. J Trauma Inj Infect Crit Care 51(6):1042–1048
Mosquera VX, Marini M, Muñiz J, Lopez-Perez JM, Gulias D, Cuenca JJ (2013) Aortic injuries in crush trauma patients: different mechanism, different management. Injury 44(1):60–65
Nagy K, Fabian T, Rodman G, Fulda G, Rodriguez A, Mirvis S (2000) Guidelines for the diagnosis and management of blunt aortic injury: an EAST Practice Management Guidelines Work Group. J Trauma Inj Infect Crit Care 48(6):1128–1143
Pang D, Hildebrand D, Bachoo P (2015) Thoracic endovascular repair (TEVAR) versus open surgery for blunt traumatic thoracic aortic injury. Pang D, editor. Cochrane Database Syst Rev. Chichester, UK: John Wiley & Sons, Ltd; 9:CD006642
Parmley LF, Mattingly TW, Manion WC, Jahnke EJ (1958) Nonpenetrating traumatic injury of the aorta. Circulation 17(6):1086–1101
Patel NH, Hahn D, Comess KA (2003) Blunt chest trauma victims: role of intravascular ultrasound and transesophageal echocardiography in cases of abnormal thoracic aortogram. J Trauma Inj Infect Crit Care 55(2):330–337
Prêtre R, Chilcott M (1997) Blunt trauma to the heart and great vessels. N Engl J Med 336(9):626–632
Prêtre R, Chilcott M, Mürith N, Panos A (1997) Blunt injury to the supra-aortic arteries. Br J Surg 84(5):603–609
Rabin J, DuBose J, Sliker CW, O’Connor JV, Scalea TM, Griffith BP (2014a) Parameters for successful nonoperative management of traumatic aortic injury. J Thorac Cardiovasc Surg 147(1):143–149
Rabin J, Harris DG, Crews GA, Ho M, Taylor BS, Sarkar R et al (2014b) Early aortic repair worsens concurrent traumatic brain injury. Ann Thorac Surg 98(1):46–51; discussion 51–52
Raptis CA, Hammer MM, Raman KG, Mellnick VM, Bhalla S (2015) Acute traumatic aortic injury: practical considerations for the diagnostic radiologist. J Thorac Imaging 30(3):202–213
Rippey JC, Royse AG (2009) Ultrasound in trauma. Best Pract Res Clin Anaesthesiol 23(3):343–362
Rosenberg JM, Bredenberg CE, Marvasti MA, Bucknam C, Conti C, Parker FB (1989) Blunt injuries to the aortic arch vessels. Ann Thorac Surg 48(4):508–513
Rousseau H, Soula P, Perreault P, Bui B, d’Othee BJ, Massabuau P et al (1999) Delayed treatment of traumatic rupture of the thoracic aorta with endoluminal covered stent. Circulation 99(4):498–504
Schwab CW, Lawson RB, Lind JF, Garland LW (1984) Aortic injury: comparison of supine and upright portable chest films to evaluate the widened mediastinum. YMEM 13(10):896–899
Semba CP, Kato N, Kee ST, Lee GK, Mitchell RS, Miller DC et al (1997) Acute rupture of the descending thoracic aorta: repair with use of endovascular stent-grafts. J Vasc Interv Radiol 8(3):337–342
Shalhub S, Starnes BW, Hatsukami TS, Karmy-Jones R, Tran NT (2011) Repair of blunt thoracic outlet arterial injuries: an evolution from open to endovascular approach. J Trauma 71(5):E114–E121
Shi Y, Tsai PI, Wall MJ, Gilani R (2015) Intravascular ultrasound enhanced aortic sizing for endovascular treatment of blunt aortic injury. J Trauma Acute Care Surg 79(5):817–821
Shorr RM, Crittenden M, Indeck M, Hartunian SL, Rodriguez A (1987) Blunt thoracic trauma. Analysis of 515 patients. Ann Surg 206(2):200–205
Simeone A, Freitas M, Frankel HL (2006) Management options in blunt aortic injury: a case series and literature review. Am Surg 72(1):25–30
Starnes BW, Lundgren RS, Gunn M, Quade S, Hatsukami TS, Tran NT et al (2012) A new classification scheme for treating blunt aortic injury. J Vasc Surg Elsevier Inc 55(1):47–54
Steenburg SD, Ravenel JG (2008) Acute traumatic thoracic aortic injuries: experience with 64-MDCT. Am J Roentgenol 191(5):1564–1569
Steenburg SD, Ravenel JG, Ikonomidis JS, Schönholz C, Reeves S (2008) Acute traumatic aortic injury: imaging evaluation and management. Radiology 248(3):748–762
Symbas JD, Halkos ME, Symbas PN (2005) Rupture of the innominate artery from blunt trauma: current options for management. J Card Surg 20(5):455–459
Takagi H, Kawai N, Umemoto T (2008) A meta-analysis of comparative studies of endovascular versus open repair for blunt thoracic aortic injury. J Thorac Cardiovasc Surg 135(6):1392–1394
Tang GL, Tehrani HY, Usman A, Katariya K, Otero C, Perez E et al (2008) Reduced mortality, paraplegia, and stroke with stent graft repair of blunt aortic transections: a modern meta-analysis. J Vasc Surg 47(3):671–675
Teixeira PG, Inaba K, Barmparas G, Georgiou C, Toms C, Noguchi TT et al (2011) Blunt thoracic aortic injuries: an autopsy study. J Trauma 70(1):197–202
Wallace GA, Starnes BW, Hatsukami TS, Sobel M, Singh N, Tran NT (2015) Intravascular ultrasound is a critical tool for accurate endograft sizing in the management of blunt thoracic aortic injury. J Vasc Surg 61(3):630–635
Waterford SD, Chou D, Bombien R, Uzun I, Shah A, Khoynezhad A (2016) Left subclavian arterial coverage and stroke during thoracic aortic endografting: a systematic review. Ann Thorac Surg 101(1):381–389
Williams DM, Simon HJ, Marx MV, Starkey TD (1992) Acute traumatic aortic rupture: intravascular US findings. Radiology 182(1):247–249
Williams DM, Dake MD, Bolling SF, Deeb GM (1993) The role of intravascular ultrasound in acute traumatic aortic rupture. Semin Ultrasound CT MR 14(2):85–90
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Berger, F.H., De Boo, D.W. (2016). Blunt Traumatic Aortic Injury. In: Scaglione, M., Linsenmaier, U., Schueller, G., Berger, F., Wirth, S. (eds) Emergency Radiology of the Chest and Cardiovascular System. Medical Radiology(). Springer, Cham. https://doi.org/10.1007/174_2016_41
Download citation
DOI: https://doi.org/10.1007/174_2016_41
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42582-5
Online ISBN: 978-3-319-42584-9
eBook Packages: MedicineMedicine (R0)