Abstract
The presence of thoracic injuries in a multisystemic trauma can highly increase patient mortality; furthermore, injuries such as “flail chest,” lung contusion, hemothorax, and pneumothorax can complicate overall case management.
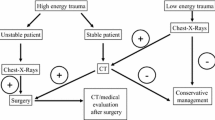
Chest-X-Ray (CXR) is the first imaging step to perform in a thoracic trauma, to highlight a possible pneumothorax, hemothorax, and other life-threatening conditions. MultiSlice Computed Tomography (MDCT) is more accurate than CXR for the evaluation of pleural injuries, although it is to be performed in stable patients only.
In this chapter, pleural abnormalities following blunt thoracic trauma and the role of CXR and MSCT will be discussed (pneumothorax, hemothorax), with a small digression about pleural drainages and the importance to recognize a possible dislocation to prevent severe complications.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Thoracic injuries are the third most common injuries in polytrauma patients, next to head and extremities’ injuries (Ahmad et al. 2013); they have an overall fatality rate of 10.1 %, highest in patients with cardiac or tracheobronchial-esophageal injuries (Ahmad et al. 2013). Furthermore, the presence of thoracic injuries in a multisystemic trauma can highly increase patient mortality. Injuries such as “flail chest,” lung contusion, hemothorax, and pneumothorax can complicate overall case management (Tocino et al. 1985). More than two-thirds of cases of blunt thoracic trauma are caused by motor vehicle collisions in developed countries. The remaining cases are due to falls or of blows from blunt objects (Ahmad et al. 2013; Cothren et al. 2007; Miele et al. 2015). Imaging plays a key role in the diagnosis of blunt thoracic trauma.
Conventional radiography is typically performed as the first imaging investigation, even if computed tomography (CT) is to be performed. Chest-X-Rays (CXR), when correctly performed, may show a tension pneumothorax, a large hemothorax, a tube and line malpositioning, and other conditions that require immediate treatment. Concerning the development of CT in this setting, several studies have shown that it may demonstrate a life-threatening disease (e.g., thoracic aortic injury) in patients with normal radiographs at the beginning (Alkadhi et al. 2004). Moreover, CT has been demonstrated to change the management in up to 20 % of chest trauma patients with abnormal initial radiographs (Błasińska-Przerwa et al. 2013). CT is more accurate than radiography for the evaluation of pulmonary contusion, and it is also valuable in the diagnosis of fractures of the thoracic spine, especially at the cervicothoracic junction, which is difficult to evaluate with conventional radiography (Brink et al. 2008, 2010; Detorakis and Androulidakis 2014 ).
In this chapter, pleural abnormalities following blunt thoracic trauma and the role of CXR and multi-slice-computed tomography (MSCT) will be discussed (pneumothorax, hemothorax), with a small digression about pleural drainages and the importance to recognize a possible dislocation to prevent severe complications.
2 Pneumothorax
The term pneumothorax (PNX) refers to the presence of air in the pleural space: it affects 60 % of patients with severe thoracic trauma, and it can be rapidly fatal even in the absence of other injuries. PNX is open when it communicates with the atmosphere through an open wound; otherwise it is a closed PNX, and it may occur due to different mechanisms of injuries: fragments of fractured rib arches may lacerate the parietal pleura layer; even in the absence of rib cage fractures, the intra-alveolar pressure, following a thoracic compression, may exceed the intrapleural pressure; hence, the passage of air into the pleural space may lacerate the visceral pleura. Finally, another possible mechanism of injury is the laceration of proximal airways. The leading causes of iatrogenic pneumothorax include central venous catheter insertion, thoracentesis, and barotrauma as a result of mechanical ventilator.
Simple PNX occurs when the pressure of the air in the pleural space does not exceed that of the atmosphere; the air pressure increases (tension PNX) when a pleural-parenchymal or bronchial injury acts as a one-way valve, namely, allowing air inflow into the pleural space on inspiration but prohibiting air outflow. Tension PNX is the most severe form of PNX, which may result in a fatal cardiopulmonary failure, and it is a common cause of death for thoracic trauma.
PNX clinical relevance depends not only on its dimensions but also on the hemodynamic conditions of patients; in fact, also a small pneumothorax can become hemodynamically significant on patients under mechanical ventilation. Massive PNX and tension PNX are life-threatening conditions and should be recognized and treated before performing any radiological evaluation. In this study, it is pointed out that the detection of a PNX requires the radiologist to give an immediate communication to the trauma leader; this communication must be written in the clinical report, as well.
Considering the numerous clinical and radiological modalities for the detection of PNX as well as the availability of treatment procedures that can be adjusted to the context and the health-care providers’ experience (such as needle decompression at the trauma setting, decompression with small-caliber drains, drainage tube placement, decompressive minithoracotomy), death due to PNX can be regarded as preventable; in trauma patients, death is caused by inadequate care and treatment rather than by the severity of the injuries sustained.
2.1 Diagnostic Imaging
Many authors have given evidence of the superiority of MSCT for the diagnosis of PNX and have recommended its employment. In most cases, the diagnosis of PNX on MSCT is easily successful, whereas the diagnosis is considered difficult on CXR (radiogram on anterior-posterior view with patient in supine position): it has been often proved that many cases of undetected PNX have been only diagnosed on MSCT (Gavelli et al. 2007). Occult pneumothorax is a pneumothorax that is only evident on MSCT (also in MSCT abdomen that in trauma patients should be always evaluated using the pulmonary window, with the scans covering the lung bases): occult PNX is recognizable in 40 % of trauma patients.
Autopsy experimental studies have highlighted that the lateral decubitus projection is the most sensitive in the detection of a PNX (88 % of all cases) in comparison with those obtained in upright position (59 %) or in clinostasis (38 %); nevertheless, they cannot be employed for polytrauma patients.
Furthermore, it must be taken into account that, while the minimum volume of air detected in the pleural space is about 50 ml in orthostasis (appreciable in lateral-apical site), at least 500 ml of air are needed for the detection of PNX in clinostasis, usually seen in an anteromedial and subpulmonary location.
The diagnostic difficulties in recognizing PNX are due to the not always excellent technical qualities of CXR and pertain to the specific semeiological characteristics that PNX takes on CXR. In orthostasis, the diagnosis of a PNX is based on the identification of the visceral pleura seen tangentially from the radiant beam (pleural line) better remarkable in the external apical/subclavian regions and on the complete absence of pulmonary pattern laterally to the “pleural line.” In clinostasis, the semeiotics of PNX is completely different (Ianniello et al. 2014).
The lateral-costal placement of PNX is, in fact, quite uncommon, as well as the indication of the “pleural line.” In fact, PNX preferably collects in the lower-anterior portion of the chest and, above all, in the anteromedial and subpulmonary site, where the flap, interposed between the base of the lung and the diaphragm, can locate both at the front and posteriorly. In cases (not uncommon) where PNX is located only in the anteromedial and subpulmonary site, the radiant beam does not tangentially detect any visceral pleural border, and the sign of the “visceral line” is not appreciable (Fig. 1).
(a) CXR: pneumothorax is located only in the anteromedial and subpulmonary site. The radiant beam does not tangentially detect any visceral pleural border, and the sign of the “visceral line” is not appreciable; (b) axial CT image shows very clearly the PNX located in the bilateral anterior-basal site
The lung presents compliance alterations (contusion, edema) that may prevent a harmonic collapse toward the ilium; the presence of lung pattern external to the supposed “pleural line” does not rule out the diagnosis of PNX.
The radiological signs to detect a PNX in clinostasis are:
-
Hyperlucency of the lower part of the chest and the upper quadrants of the abdomen (Fig. 2)
-
Deep sign of the lateral pleural sinus (the deep sulcus sign) (Fig. 3)
-
Double-diaphragm appearance
-
Sharp appearance of the diaphragmatic outline (Fig. 4)
Fig. 4 (a) CXR image: bilaterally appreciable is the sharp appearance of the diaphragmatic outline; also evident is a clear demarcation of the profile of the aortic arch and the cardiac silhouette. (b) Axial CT scan and (c) coronal reconstruction demonstrate the presence of PNX localized in the bilateral anteromedial site
-
Sharpness of the cardiophrenic fat pad
-
Sharpness of the inferior surface of the lung
-
High visibility of the pleural surface of the lung (more frequent in apical position)
Air can, also, separate the edges of the heart, aorta, and vena cava that take an unusual sharp appearance. The air, collected in the posteromedial pleural recess, can be recognized as radiotransparent paraspinal line, alongside the descending aorta and in the posterior costophrenic sulcus. It is essential to carefully inspect the lower lobes of the lung and the upper abdomen to avoid missing such signs. In general, if small flaps of PNX, unrecognized on AP view, have no clinical relevance, they may rapidly expand in intubated patients on positive-pressure ventilation, putting the patient’s life at risk. In such a scenario, the radiographic evidence of rib fractures and homolateral subcutaneous emphysema are considered a sign of PNX even in the absence of sharp intrapleural gas folds.
3 Tension PNX
Tension PNX is an emergency clinical condition that requires an immediate treatment, being associated with a reduction of cardiac filling and compression of the homolateral lung. About one-third of the patients with unrecognized PNX progress into a tension PNX.
If the diagnostic evidence of a simple PNX must be communicated to the trauma leader in real time (and written in the report), the same is even true for the diagnosis of tension PNX (Mirvis et al. 2004, 2005).
3.1 Diagnostic Imaging
The radiological diagnosis of PNX can be guided through the following signs:
-
Contralateral dislocation of the mediastinum (Figs. 5 and 6)
Fig. 5 -
Flattening/inversion of the diaphragm (Fig. 7)
-
Extension of the intercostal spaces (Fig. 7)
-
Flattening of the cardiac profile (Fig. 8)
The mediastinal shift is not a specific sign of tension PNX because it may be visible, to some extent, also in simple PNX; on the other hand, the flattening of the cardiac profile may be the sign better related to the cardiovascular and respiratory distress that markedly characterizes the tension PNX. If tension PNX is persistent despite the correct functioning of the drainage, it is essential to rule out any injury of the main airways.
4 Hemothorax
In polytraumatized patients with blunt chest trauma, pleural effusion is present in approximately 30–50 % of cases, and it is usually hematic in nature (hemothorax) (Brooks et al. 2004).
However, in the acute stage, it is also possible to detect simple serous effusions (due to a reduction of the respiratory mechanics and pleural reabsorption) often associated with atelectasis or homolateral chest wall injuries that reduce the respiratory excursion. On the other hand, it is quite occasional the detection of chylous effusion, due to the rupture of either the thoracic lymphatic ducts (thoracic duct) or of the bile duct, as a result of biliopleural fistula formation that is more common in penetrating trauma.
Bleeding in the pleural cavity often occurs some hours after the trauma; it is sometimes bilateral, and it is often associated with a PNX. The causes responsible for a hemothorax include lacerations of the intercostal vessels, pulmonary contusions, pleural and pulmonary lacerations, and injuries to the diaphragm; iatrogenic lesions, for example, those following a central venous catheter, are also possible causes.
The management of hemothorax depends on its initial quantity, on the amount of blood flow, and on the health condition of the patient.
The initial, usually decisive treatment is the placement of a tube thoracostomy. Patients, who, as soon as the drainage is inserted, evacuate more than 1500 cc, need a surgical or endovascular control of the bleeding.
A hemothorax associated with contusion is usually self-limiting, whereas it may be massive and protracted, when it is associated with pulmonary lacerations or mediastinal lesions.
Venous hemorrhages are self-limited and without mass effect, whereas arterial hemorrhages are under pressure, and they may trigger a significant compression of the pulmonary parenchyma, mediastinum, and heart.
The initial recesses of the pleural cavity filled with blood effusion are declivitous; they can vary according to the decubitus, whereas, with the progressive filling of the pleural cavity, blood is invariably collected in the lateral pleural spaces over the apex of the lung (apical cap): they are very large pleural effusions, in the order of about 800–1200 cc.
4.1 Diagnostic Imaging
In orthostatic position, the most declivitous part of the pleural space is the subpulmonary space; the radiological sign is an apparent elevation of the diaphragm which appears flattened at its medial margins. When at least 200 cc of effusion are collected, the fluid, visible tangentially to the X-ray beam, has a meniscus shape and obliterates the lateral costophrenic sulcus.
On the contrary, in supine patient, the blood collects posteriorly and along the posterior pleural space; on CXR, it is acquired “face to face” (on the frontal view), not tangentially to the radiant beam. For this reason, the “formation” of meniscus sign is not usually visible, and the radiological sign is often only a homogeneous increased density in the basal medial hemithorax with visualization of the parenchymal markings associated with the obliteration of the lateral costophrenic recess. In clinostatic position, neither pleural effusions below 200–300 cc nor massive effusions collected posteriorly can usually be detected. The contralateral mediastinal shift indicates a hemithorax under pressure, probably due to an arterial bleeding (Fig. 9). Atypical radiological appearances include loculated collections that may mimic a mass in the interlobar fissures or in the mediastinal pleura and lobulated margins of the effusion which is collected along the pleural surface, due to the advanced coagulation process, however rather rare in the acute stage.
The identification of pleural effusion as well as its diversification from abdominal effusion is quite easy to acquire on MSCT, thanks to the use of multiplanar reconstruction (MPR). The density of a hemothorax generally varies from 35 to 70 HU, depending on the hematocrit, the mixture of other fluids (serous) in the pleural space, and the potential clot formation.
The presence of a liquid-liquid level may further enforce the diagnosis for a blood effusion: the blood, in fact, has a layered appearance according to its degree of coagulation (“hematocrit sign”).
Occasionally, an active extravasation can be visible and it should be carefully observed, suggesting urgent hemostasis through surgical or endovascular intervention (Fig. 10).
Generally, active extravasation refers to any passage of contrast medium out of the arteries, veins, bowel, and urinary tract. Active extravasation is seen in a minority of trauma patients, in whom MSCT shows a hemothorax, whose detection is more accurate with a dual-phase protocol (Fig. 11). The classic pattern of active extravasation at dual phase is a “jet” or focal area of hyperattenuation within a hematoma that, between the initial and the delayed images acquisition, shows a visible enlargement (Fig. 12).
This finding is indicative of significant bleeding and must be quickly communicated to the clinician, since it is an indicator of the need for surgical or endovascular intervention (Hamilton 2008; Kaewlai et al. 2008; Kalsow et al. 2013).
The active extravasation may be recognized when the attenuation is greater than clotted blood presenting a density of about 70–90 HU: most active extravasations present an attenuation greater than 100 HU. To obtain an optimal scanning of the active extravasation in polytrauma patients, it is suggested the use of 150 mL of contrast medium 300 mgl/l, administered at a rate of 3.5 ml/s with the beginning of the acquisition about 1 min after the start of the bolus; the delay time is slightly longer than that used in standard arterial acquisition and its purpose is to assure an optimum enhancement of the parenchymal organs. Furthermore, a delayed acquisition (for example, at a rate of 5 min) can be performed with a low-flow technique to complete the semeiotic evaluation of the findings (Lomoschitz et al. 2003, Mayberry 2000; O’Connor et al. 2009).
5 Appendix: Pleural Drainages
The placement of one or more thoracostomy tubes represents the standard procedure for treating PNX and hemothorax. The tube bore size varies from 10 to 40 F, depending on the thickness of the fluid to be drained and the physician’s preference; the course’s tube, inserted in the midaxillary line, is anterosuperior for the PNX drainage and posteroinferior for the evacuation of the hemothorax (McDermott et al. 2012). The chest tube is appropriately placed when its apex is within the pleural space, namely, between the parietal and visceral pleurae. The positioning procedure can be frequently considered rather safe; however, the critical conditions of polytraumatized patients are often associated with the malfunctioning of the drainage system: the chest tube does not drain air or fluid if connected to an aspiration device, or the radiological follow-up shows the persistence of a PNX or hemothorax. Causes of malfunctioning include kinking, blocked drain due to clot formation, and tube malposition (MP). Malposition of the drain is the most common complication in an emergency; it is placed in intrafissural and intraparenchymal apices, in the mediastinum, or in abdominal (through a diaphragmatic tear) and extrapulmonary subcutaneous tissues. The MP of the chest tube results in a longer length of hospital stay and risk of infectious complications. Moreover, the intraparenchymal drains may result in pulmonary abscess or may cause parenchymal hemorrhage; besides, the delay in the evacuation of hemothorax can lead to empyema (Pastore Neto et al. 2015).
The clinical recognition of MP is difficult. The CXR is usually performed as a follow-up examination, following the insertion of the drainage system, to assess the parenchymal expansion and the reduction of PNX/hemithorax flap as well as to identify the apex of the drainage tube; however, the reliability of MP detection may be considered poor and limited to ordinary cases (25 % of all cases). The identification of MP is easy on CT, with an incidence between 15 and 26 % (Corcoran et al. 2015).
A PNX is persistent when it is visible despite the drainage placement: a persistent PNX may be hypertensive, and its presence must be communicated to the team leader immediately.
References
Ahmad T, Ahmed SW, Soomro NH et al (2013) Thoracoscopic evacuation of retained post-traumatic hemothorax. J Coll Physicians Surg Pak 23:234–236
Alkadhi H, Wildermuth S, Desbiolles L et al (2004) Vascular emergencies of the Thorax after Blunt and Iatrogenic trauma: multi-detector row CT and three-dimensional imaging. Radiographics 24:1239–1255
Błasińska-Przerwa K, Pacho R, Bestry I (2013) The application of MDCT in the diagnosis of chest trauma. Pneumonol Alergol Pol 81:518–526
Brink M, Deunk J, Dekker HM et al (2008) Added value of routine chest MDCT after blunt trauma: evaluation of additional findings and Impact on patient management. AJR Am J Roentgenol 190:1591–1598
Brink M, Deunk J, Dekker HM et al (2010) Criteria for the selective use of chest computed tomography in blunt trauma patients. Eur Radiol 20:818–828
Brooks A, Davies B, Smethhurts M et al (2004) Emergency ultrasound in the acute assessment of haemothorax. Emerg Med J 21:44–46
Corcoran JP, Acton L, Ahmed A et al (2015) Diagnostic value of radiological imaging pre- and post-drainage of pleural effusions. Respirology. doi:10.1111/resp.12675
Cothren CC, Moore EE, Hedegaard HB et al (2007) Epidemiology of urban trauma deaths: a comprehensive reassessment 10 years later. World J Surg 31:1507–1511
Detorakis EE, Androulidakis E (2014) Intercostal lung herniation- the role of imaging. J Radiol Case Rep 8:16–24
Gavelli G, Napoli G, Bertaccini P et al (2007) Imaging of thoracic injuries. In: Marincek B, Dondelinger RF (eds) Emergency radiology – imaging and intervention. Springer, Berlin Heidelberg, pp 155–178
Hamilton JD, Kumaravel M, Censullo ML et al (2008) Multidetector CT evaluation of active extravasation in blunt abdominal and pelvic trauma patients. Radiographics 28:1603–1616
Ianniello S, Di Giacomo V, Sessa B, Miele V (2014) First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. Radiol Med 119: 674–680
Kaewlai R, Avery LL, Asrani AV et al (2008) Multidetector CT of blunt thoracic trauma. Radiographics 28:1555–1570
Kalsow S, Wigle R, Johnson LW et al (2013) Delayed traumatic lung herniation. J La State Med Soc 165:163–165
Lomoschitz FM, Eisenhuber E, Linnau KF et al (2003) Imaging of chest trauma: radiological patterns of injuries and diagnostic algorithms. Eur J Radiol 48:61–70
Mayberry JC (2000) Imaging in thoracic trauma: the trauma surgeon’s perspective. J Thorac Imaging 15:76–86
McDermott S, Levis DA, Arellano RS (2012) Chest drainage. Semin Intervent Radiol 29:247–255
Miele V, Di Giampietro I, Ianniello S, Pinto F, Trinci M (2014) Diagnostic imaging in pediatric polytrauma management. Radiol Med 120:33–49
Mirvis SE (2004) Diagnostic imaging of acute thoracic injury. Semin Ultrasound CT MR 25:156–179
Mirvis SE (2005) Imaging of acute thoracic injury: the advent of MDCT screening. Semin Ultrasound CT MR 26:305–331
O’Connor JV, Byrne C, Scalea TM et al (2009) Vascular injuries after blunt chest trauma: diagnosis and management. Scand J Trauma Resusc Emerg Med 17:42
Pastore Neto M, Resende V, Machado CJ et al (2015) Associated factors to empyema in post-traumatic hemotorax. Rev Col Bras Cir 42:224–230
Tocino IM, Miller MH, Fairfax WR (1985) Distribution of pneumothorax in the supine and semirecumbent critically ill adult. AJR Am J Roentgenol 144:901–905
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Miele, V., Buquicchio, G.L., Piccolo, C.L., Stasolla, A., Ianniello, S., Brunese, L. (2016). Injuries of the Pleural Spaces. In: Scaglione, M., Linsenmaier, U., Schueller, G., Berger, F., Wirth, S. (eds) Emergency Radiology of the Chest and Cardiovascular System. Medical Radiology(). Springer, Cham. https://doi.org/10.1007/174_2016_29
Download citation
DOI: https://doi.org/10.1007/174_2016_29
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42582-5
Online ISBN: 978-3-319-42584-9
eBook Packages: MedicineMedicine (R0)