Abstract
Pregnant women, fetuses, and newborns are particularly vulnerable patient populations. During pregnancy, the body is subject to physiological changes that influence the pharmacokinetics and pharmacodynamics of drugs. Inappropriate dosing in pregnant women can result in sub-therapeutic or toxic effects, putting not only the pregnant woman but also her fetus at risk. During neonatal life, maturation processes also affect pharmacokinetics and pharmacodynamics of drugs. Inappropriate dosing in newborns leads not only to short-term complications but can also have a negative impact on the long-term development of infants and children. For these reasons, it is crucial to characterize physiological changes in pregnant women, describe placental transfer kinetics of drugs, and describe physiological changes related to the transition from intrauterine to extrauterine life and maturation processes in preterm and term neonates. Quantitative pharmacological approaches such as pharmacometric and physiologically-based modeling and model-based simulations can be useful to better understand and predict such physiological changes and their effects on drug exposure and response. This review article (1) gives an overview of physiological changes in pregnant women, their fetuses, and (pre)term neonates, (2) presents case studies to illustrate applications of new modeling and simulation approaches, and (3) discusses challenges and opportunities in optimizing and personalizing treatments during pregnancy and neonatal life.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The core goal of pediatric clinical pharmacology is to improve care through effective and safe use of drugs in fetuses, neonates, infants, children, and adolescents. Studying the effectiveness and safety of drugs in pregnant women and children by conducting clinical trials is less straightforward as compared to performing these in adults due to practical and ethical concerns. This review will present an overview of the physiological changes in pregnant women, their fetuses, and (pre)term neonates with the integration of pharmacometrics in pediatric clinical pharmacology resulting in the development of evidence-based pharmacotherapy during pregnancy and neonatal life.
Physiological changes during pregnancy can influence the disposition of various drugs. Inappropriate dosing in pregnant women can result in sub-therapeutic or even toxic effects, putting not only the pregnant woman but also her fetus at risk (Moore et al. 2002). After birth, the newborn is as well subject to rapid physiological changes related to the transition from intrauterine to extrauterine life and maturational processes affecting the pharmacokinetics and pharmacodynamics of administered drugs (Kearns et al. 2003). Incorrect dosing in neonates results not only in short-term complications but can also have a negative impact on the long-term development of infants and children (Allegaert and Anker 2015). As a consequence, it is very important to characterize these physiological changes in pregnant women, investigate the placental transfer of drugs, and describe the physiological changes and corresponding consequences related to maturation in preterm and term newborns.
Currently, there are various approaches to assess these challenges, such as pharmacometric and physiologically-based modeling together with model-based simulations, which can help us characterize relevant physiological changes and their effects on drug exposure and response during pregnancy and neonatal life. Although there are still challenges to overcome, such as the implementation of these approaches in daily clinical practice, a lot of progress has been made.
2 Understanding the Impact of Physiological Changes on Pharmacotherapy During Pregnancy and Neonatal Life
In the next paragraphs, we will highlight the influence of physiological changes on the pharmacotherapy for the pregnant woman and her unborn fetus and for the newborn during the neonatal period (first 28 days of life).
2.1 Pregnancy and Pharmacotherapy: Something to Worry About?
During pregnancy, women take a variety of medications (either prescribed or over the counter) which can have negative impacts on the pregnant woman and her unborn child. Antenatal medication use during pregnancy has increased over the last three decades (Mitchell et al. 2011). On the other hand, recent study showed that women of child-bearing age in Switzerland have high general health awareness, and when they become pregnant, most of them refrain from using pain killers (Bornhauser et al. 2017). Surveys about their medication use have illustrated that the percentage of pregnant women who took pain killers once a week to several times a week was about half of that in nonpregnant women (25% vs 50%). Of note, in 67% of pregnant women using pain killers, these were prescribed by a physician, as compared to 35% in nonpregnant women (Bornhauser et al. 2017).
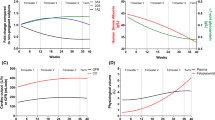
Pregnancy affects various physiological processes and alters the body composition of the pregnant woman. These changes can affect the pharmacokinetics of drugs and should therefore be taken into account when prescribing drugs and may even require dosing adjustments to ensure appropriate treatment (Dallmann et al. 2018a). A recent review investigated the alterations in pharmacokinetics during pregnancy studying 121 different medications based on 198 studies in pregnant women (Pariente et al. 2016). Enhanced elimination, resulting in decreased drug exposure at a given dose, was one of the main conclusions. Alterations in drug absorption (ka) are caused by altered bioavailability and delayed time to reach peak levels after oral administration, which are due to decreased gastrointestinal motility and increased gastric pH (Fig. 1) (Loebstein et al. 1997). For hydrophilic drugs, the volume of distribution (Vd) is increased because of increased total body water and plasma volume, whereas Vd for hydrophobic drugs is increased because of a larger fat compartment. Clearance (CL) of drugs is influenced by many processes such as altered glomerular filtration rate and an adjusted cardiac output (Pariente et al. 2016). Furthermore, diminished plasma albumin concentrations during pregnancy may increase free, and therefore active, drug concentrations associated with a potential increase in drug activity, depending on the physiochemical characteristics of a given drug (Pariente et al. 2016). Unfortunately, for a majority of drugs used during pregnancy, information regarding pharmacokinetic (PK) changes and related effects on safety and efficacy is still lacking.
Schematic overview representing physiological changes and their corresponding impact on pharmacokinetics in pregnant women, their fetus, and newborns. Data retrieved from literature (Anderson 2005; Bonner et al. 2015; Hines 2008; Kearns et al. 2003; Koren 1997; Morton and Brodsky 2016; Pariente et al. 2016; van den Anker et al. 2018; Zhang et al. 2017; Zhang and Unadkat 2017). ADME absorption, distribution, metabolism, and excretion, ka absorption rate, Vd volume of distribution, CL clearance, GA gestational age
Physiology-based pharmacokinetics (PBPK) models are increasingly utilized to characterize changes in pharmacokinetics during pregnancy (Dallmann et al. 2018a). In such mechanistic models, physiological parameters (e.g. organ volumes, glomerular filtration rate) are combined with drug-specific parameters (e.g. lipophilicity, molecular mass), and this ensures the assessment of valuable insights into the PK profiles of drugs in this specific population (Hartmanshenn et al. 2016). The prediction of drug exposure could contribute to the adjustment of dosing regimen for drugs prescribed in pregnant women. PBPK modeling can also be deployed to understand effects of concomitantly interacting drugs, which is often the case for HIV-infected women because of their combination antiretroviral therapy. The following example elegantly shows the practical utility of PBPK modeling in the pregnant population to ensure an optimal and practical dose. A recently developed PBPK model predicted a decrease in darunavir/ritonavir exposure and therefore efficacy during pregnancy when taking 800/100 mg once daily. When the dosing regimen was adjusted to 600/100 mg twice daily, the lack in exposure was compensated (Colbers et al. 2016; Ke et al. 2018).
In addition to acquire valuable insights in the pharmacokinetics and pharmacodynamics of drugs during pregnancy, it is of equal importance to understand the physiology of pregnancy-related diseases, for example, with the aid of biomarkers. New biomarkers can help to understand the cause, diagnosis, progression, and treatment of a disease (Mayeux 2004). Hypertensive disorders such as preeclampsia are a major contributor to maternal mortality worldwide (Steegers et al. 2010; Widmer et al. 2015). A lot of research has been done in the field of translational biomarkers which consequently has improved our understanding of preeclampsia and helped us better define the diagnosis of this pregnancy-related disease (Karumanchi 2016). Preeclampsia is diagnosed when there is a combination of increased proteinuria (≥300 mg in 24 h) and pregnancy-induced hypertension (diastolic blood pressure ≥90 mmHg) (Evers et al. 2018; Steegers et al. 2010). Various placental anti-angiogenic markers have been investigated, such as soluble endoglin (sEng) and soluble fms-like tyrosine kinase 1 (sFlt-1) that both can cause endothelial dysfunction (Maynard and Karumanchi 2011; Venkatesha et al. 2006). Levels of sEng are correlated with disease severity in preeclamptic pregnant women, together with an increase in sFlt-1 levels (Venkatesha et al. 2006). Furthermore, women suffering from preeclampsia showed decreased levels of free (unbound) serum placental growth factor (PIGF) and free vascular endothelial growth factor (VEGF) before developing clinical signs (Levine et al. 2004). Maternal serum neutrophil gelatinase-associated lipocalin (NGAL) levels are significantly increased in preeclamptic women, and the renal marker cystatin C measured at the end of the third trimester is a predictor of preeclampsia (Artunc-Ulkumen et al. 2015; Risch et al. 2017). In a longitudinal prospective study, it was found that neurofilament light (NfL) concentrations were higher in women with preeclampsia as compared to women who do not develop preeclampsia. Elevated levels of NfL are increasingly recognized as a measure of acute or chronic neuroaxonal damage, and NfL can be used as a predictive value for preeclampsia, especially in women older than 36 years (Evers et al. 2018). New attempts aim at combining biochemical with biophysical markers for a more precise diagnosis of preeclampsia (Kumer et al. 2018). Despite the numerous results, it is important to note that the biomarkers that are listed are not specific for preeclampsia and are also used outside of pregnancy. It is therefore still necessary to search for specific markers and interventions (Huppertz 2018).
2.2 Drug Exposure in the Fetus: Does the Placenta Act as a Barrier?
Contrary to what was assumed decades ago, the placenta does unfortunately not serve as a barrier that prevents drugs from reaching the fetus (Etwel et al. 2014). Drug exposure of the pregnant woman can have an impact on the unborn child. Therapeutic drugs are prescribed to prevent or treat conditions that develop during pregnancy and to guarantee the health of the woman, although in some cases, the target of the treatment is the fetus, as is the case with the prevention of HIV transmission (Kesho Bora Study Group 2011). Regardless whether the fetus is the actual target of pharmacological therapy, the fetus is exposed to almost every drug taken by the pregnant woman. It needs no clarification that the ability to evaluate the fetal exposure to drugs, either their efficacy but most importantly, their risk of toxicity, is imperative.
As it is currently impossible to study drug exposure prior to birth and even at the time of birth, the assessment of fetal exposure to drugs is limited to a single measurement of umbilical cord plasma concentration, which unfortunately does not reflect fetal drug exposure (Zhang et al. 2017). A recent review showed that fetal serum albumin concentrations, in contrast to serum albumin concentrations of pregnant woman, increase with advancing gestational age (GA), although they remain relatively low compared to adult values (Zhang et al. 2017). Fetal serum albumin levels reach 22.1 g/L at week 20 of gestation and 38.3 g/L at week 40 of gestation, a 1.73-fold increase (Zhang et al. 2017). Alpha1-glycoprotein, one of the major drug-binding proteins, was increased from 0.068 g/L at 20 weeks of gestation to 0.23 g/L at 40 weeks of gestation. In addition, the placental transfer layer is the thinnest just before birth, reducing the expression of certain efflux transporters such as P-glycoprotein. Therefore, the transfer of drugs and the fetal exposure may be maximal at term, as compared to earlier gestational ages (Fig. 1) (Etwel et al. 2014). A 29.4-fold increase in the large intestinal volume between 20 and 40 weeks of gestation has been demonstrated (Zhang et al. 2017). Additionally, it has been shown that hepatic organogenesis begins from the fetal mesoderm and endoderm during the fourth week of gestation and transcription of hepatic enzymes involved in drug metabolism has been detected at 8–10 weeks of gestation (Hines 2008). Focusing on the volume of the kidney in a period between 20 and 40 weeks of gestation, the volume increased from 3.39 to 31.21 mL (Zhang et al. 2017). During pregnancy, the homeostasis is assigned to the placenta, and the main task of the fetal kidney is the excretion of urine (hypotonic) as a major component of the amniotic fluid. This might explain why the glomerular filtration rate in the fetus is low, even at the end of gestation (Fig. 1) (Saint-Faust et al. 2014).
Because of ethical and practical constraints of performing clinical trials in this subpopulation, PBPK modeling could provide mechanistic understanding of the fetal drug exposure and might be able to predict the drug exposure during the entire pregnancy until birth. Several research groups have tried to quantify the placental drug transfer to the fetus. Although many of the approaches are substance-specific and therefore cannot be used for other compounds, these are valuable contributions (Abduljalil et al. 2018; Schalkwijk et al. 2018; Zhang et al. 2017; Zhang and Unadkat 2017). We expect that in the near future, more knowledge will be gained in fetal pharmacotherapy and that PBPK modeling will contribute to this.
A recent publication provided understanding on the exposure of ceftazidime in both the pregnant woman and the fetus by the development of a population PK model (Dallmann et al. 2018b). Ceftazidime has been frequently used in pregnant women to treat intrauterine or urinary tract infections. This antibiotic is hydrophilic causing it to mainly distribute into tissues with high water content (e.g. kidneys), and it is purely eliminated by glomerular filtration. Since ceftazidime crosses the placenta, concentrations in the plasma of the pregnant woman and in amniotic fluid are similar. This PK model has provided insights on the pharmacokinetics of ceftazidime in pregnant women and newborns, low drug clearance during the first days of life of newborns is most likely due to the reduced number of perfused glomeruli and reduced renal blood flow (Dallmann et al. 2018b).
Performing clinical trials in newborns is especially cumbersome, not only because of ethical considerations but also due to practical challenges such as limited amount of blood and the corresponding inability to collect multiple samples. Currently, biomarkers to assess fetal drug exposure gain attention; examples are neonatal hair tests or placental corticotrophin-releasing hormone (CRH) levels (Koren et al. 2008; Manokhina et al. 2017; Stout et al. 2015). The ability to diagnose the exposure during pregnancy after birth by neonatal hair has evolved. In neonates, hair grows during the last trimester of pregnancy. A positive neonatal hair test (for cocaine, opioids, cannabinoids, etc.) can reflect fetal exposure, even long after the pregnant woman became aware of her pregnancy, making hair an easily available carrier for biomarkers of maternal drug dependence (Etwel et al. 2014; Koren et al. 2008). Assessing the CRH levels during the third trimester of pregnancy can provide insights on the risk of obesity later in life. Elevated placental CRF has been shown to be associated with catch-up growth, which has been shown to be a prognostic factor for increased metabolic activity and, therefore, obesity (Stout et al. 2015).
2.3 Neonatal Life and Pharmacotherapy: Do We Need New Dosing Strategies?
From a pharmacological point of view, neonates are considered as a separate subpopulation, different from small children and adults (Kearns et al. 2003). In order to provide evidence-based and tailored dosing recommendations, it is clear that we first need to have a clear understanding of the physiological changes that occur during the neonatal period.
Levels of gastric pH after birth are unclear because of contradicting information (Kearns et al. 2003; Koren 1997; van den Anker et al. 2018). An acidic gastric pH has been observed in preterm neonates, but oral ingestion of acid-buffering milk might result in an increase in gastric pH values. Gastric emptying is an important factor for intestinal drug absorption and appears not to be driven by age, but by type of food intake (Bonner et al. 2015). The extracellular and total body water compartments differ vastly between newborns, infants, children, adolescents, and adults (Kearns et al. 2003; Ku and Smith 2014). This causes water-soluble drugs (e.g. aminoglycosides) to distribute into a larger physiological (extracellular) space in neonates; in order to reach effective drug exposure, they require higher dosages (Fig. 1). The distribution of drugs in the central nervous system is different in newborns versus children and adults. Due to decreased protein binding, a higher ratio of cerebral to systemic blood flow, and a higher relative brain weight, the concentrations in brain are likely to be higher in newborns (Ku and Smith 2014; Seyberth and Kauffman 2011). Drug-metabolizing enzymes play an important role in the transformation of xenobiotics. Overall, three different developmental trajectories can be observed according to the ontogeny of drug-metabolizing enzymes (Hines 2008). During gestation, group 1 of these drug-metabolizing enzymes become highly active but are only expressed at low levels after birth (e.g. CYP3A7). The second group consists of enzymes which are expressed at constant levels during gestation and after birth. In the last group, the enzymes are present which expression is observed within the first 2 years of life (Hines 2008). The renal clearance increases with advancing gestational age, postnatal age, and body weight (Kearns et al. 2003). The creatinine clearance remains the best measurement of the assessment of GFR in this population, although it is widely known that assessment of serum creatinine levels during the first days after birth is rather a reflection of the mother’s renal function than that of the newborn, since creatinine is easily transferred across the placenta (Kastl 2017). At birth, which is known to be an accelerator for postnatal maturation of renal function, the vascular resistance decreases, and an increase in cardiac output and renal blood flow is observed, which will alter the GFR (Saint-Faust et al. 2014; Sulemanji and Vakili 2013). The renal tubules are not yet structurally or functionally mature at birth and lead to an activity that is approximately 20% of the adult value. By 7–8 months the adult tubular secretion values will be attained (Hines 2008). Although creatinine clearance is currently the best way to determine the renal function, it is probably not the most accurate method to use in newborns. A new renal biomarker such as cystatin C, a protein which is freely filtered by the glomerulus, may reflect the GFR more closely in preterm infants (Saint-Faust et al. 2014). Beta-trace protein is another possible renal marker which does not cross the placental barrier and is subject to increased attention as new indicator of GFR and renal function (Kastl 2017; Saint-Faust et al. 2014).
Integrating pharmacological expertise combined with clinical knowledge on physiological changes provides a strong foundation for innovative and new evidence-based dosing recommendations which are highly necessary for neonates as they are being considered the last therapeutic orphans.
If born prematurely, apnea is often observed due to immaturity of the central nervous system and is primarily treated with caffeine. Although this drug is commonly used across many neonatal intensive care units by a standard dosing regimen consisting of a loading dose (20 mg/kg) followed by a maintenance dose (5 mg/kg/day), not much is known about the effect of the increasing caffeine clearance after birth. Recent research has shown that a higher maintenance dose is required in preterm neonates with apnea to maintain caffeine concentrations above 15 mg/L after the first week of life (Koch et al. 2017). Gentamicin, a widely used antibiotic where the pharmacokinetic understanding has increased over the past years, can be used as another illustration. Despite the increased knowledge, this has resulted in considerable variability in dosing regimen recommendations with respect to dose, dosing interval, and patient characteristics. Model-based simulations for this antibiotic treatment in neonates illustrated that in order to attain an effective peak concentration of 10 mg/L, a dose of 7.5 mg/kg should be administered using an extended dosing interval based on gestational and postnatal age to reduce the risk of renal toxicity (van Donge et al. 2018).
During the first days after birth, newborns will lose body fluids and fat resulting in an initial weight loss. When this weight loss becomes excessive (>10% of birth weight), the risk for serious clinical complications increases (Wilbaux et al. 2016). The use of weight monographs belongs to the current practice, and if a newborn loses 5% of its body weight during the first day of life, this is seen as a critical sign. In 2016, a semi-mechanistic model characterized the weight changes in healthy neonates and quantified key factors (maternal and neonatal) influencing individual weight profiles during the first 7 days of life. It was illustrated that birth weight increases more with advancing gestational age and that boys weigh more than girls at birth. In addition, it was showed that weight gain is influenced by gestational age and that birth weight increases with the maternal age (Wilbaux et al. 2016).
3 Optimize and Personalize Pharmacotherapy During Pregnancy and Neonatal Life
In this new era which is highlighted by technology and innovative approaches, it should not be the case that pregnant women and their newborns are still dependent on off-label drug use. By incorporating knowledge on the physiological changes that happen during these life-changing periods, we can assess the influence on pharmacokinetic profiles and adjust dosing recommendations, ensuring a safe and effective treatment.
Only in the rare circumstance that there is similarity between adults and infants in disease, the mechanism of action of the drug, and the PK/PD relationships, it is justified and allowed to extrapolate the pediatric dose from adult dosages (Manolis and Pons 2009). Otherwise it is required to address all these components before extrapolating pediatric dose from adult standard of care.
Modeling and simulation can not only be applied in order to gain insights in the PK of drugs in this special population; it can also support and optimize the design of pediatric studies. When designing a new pediatric pharmacokinetic/pharmacodynamic study, it is important to know how many samples per patient are required, what the best sampling times are, and how many patients are needed to obtain a statistically powered estimation of the PK/PD parameters. After obtaining clinical data, the first step for PK/PD model-based guidance is to select the appropriate target in the population of interest, such as a desired plasma concentration, target exposure (area under the curve, AUC), time above target exposure, or other measure matrices. Thereafter, one can define the dosage regimen to best achieve this target while taking into account various factors which influence the disposition of the drug (demographic characteristics such as gestational age, weight, or postnatal age).
Development of pregnancy PBPK models makes it possible to assess drug exposure in all trimesters and investigate multiple dosing strategies. Although over the recent years a lot of progress is made with pregnancy PBPK models, knowledge gaps still remain. An integrated fetomaternal PBPK model would be able to examine fetal drug therapy during pregnancy. In order to develop such a complex model, quantitative information on system-specific parameters need to be incorporated into the pregnancy PBPK model, and the characterization of the fetal system in terms of enzyme and transporter tissue abundance remains challenging (Dallmann et al. 2018a). In addition, obtaining data on fetal drug exposure for the evaluation of the fetal PBPK model continues to be cumbersome.
One of the greatest opportunities of using these novel technologies to optimize and personalize pharmacotherapy is at the same time one of the greatest challenges, that is to say, the integration of these research-based models in easily accessible software tools which can become part of daily clinical practice.
Neoweight is an example of such a user-friendly online prediction tool which can forecasts the individual weight changes during the first week of life, based on three weight measurements and standard characteristics of the newborn, and can be found at http://neoweight.mashframe.com (Wilbaux et al. 2016). We hope that in the near future, more validated, user-friendly tools will be developed and integrated in clinical practice. It is rather worrisome that these innovative and novel approaches are being developed in order to ensure safe and effective treatment for the patient but will never fulfill this goal because of problems with translation, implementation, and lack of easy accessibility.
Initiatives to build national and international collaborative networks to facilitate clinical trials and collection and sharing of data are necessary. The Swiss Research Network of Clinical Pediatric Centers (SwissPedNet) and the Swiss Research Center for Pediatric Pharmacology and Pharmacometrics (SwissPedPha) are examples of such national initiatives. In 2012, this research network of pediatric hospitals has been created and has the common goal to facilitate, coordinate, and conduct clinical trials in all pediatric disciplines. Another initiative is the Dutch Center for Pharmacotherapy for Children (NKFK) which aims to improve the quality and safety of pharmacotherapy in children and focuses on improving the provision of information about the use of drugs in children.
4 Conclusion
The characterization of physiological changes in pregnant women, the description of placental transfer kinetics of drugs, the identification of physiological changes related to the transition from intrauterine to extrauterine life, and the characterization of maturation processes in preterm and term neonates are essential in order to ensure safe and effective treatment in both the pregnant women and her fetus or newborn.
Once dosing recommendations based on new biomarkers, pharmacometric approaches, and/or PBPK predictions have been validated in clinical trials, results can be incorporated in clinical practice. Bedside decision support tools should be developed to facilitate optimizing and individualizing treatment strategies in vulnerable patient populations such as pregnant women and their fetuses and newborns. Quantitative pharmacology and pharmacometric approaches have the potential to further personalize and enhance patient care allowing safe and efficacious use of drugs during pregnancy and neonatal life.
References
Abduljalil K, Johnson TN, Rostami-Hodjegan A (2018) Fetal physiologically-based pharmacokinetic models: systems information on fetal biometry and gross composition. Clin Pharmacokinet 57:1149–1171
Allegaert K, Anker JN (2015) Adverse drug reactions in neonates and infants: a population-tailored approach is needed. Br J Clin Pharmacol 80:788–795
Anderson GD (2005) Pregnancy-induced changes in pharmacokinetics. Clin Pharmacokinet 44:989–1008
Artunc-Ulkumen B, Guvenc Y, Goker A, Gozukara C (2015) Relationship of neutrophil gelatinase-associated lipocalin (NGAL) and procalcitonin levels with the presence and severity of the preeclampsia. J Matern Fetal Neonatal Med 28:1895–1900. https://doi.org/10.3109/14767058.2014.972926
Bonner JJ, Vajjah P, Abduljalil K, Jamei M, Rostami-Hodjegan A, Tucker GT, Johnson TN (2015) Does age affect gastric emptying time? A model-based meta-analysis of data from premature neonates through to adults. Biopharm Drug Dispos 36:245–257
Bornhauser C, Quack KL, Seifert B, Simões-Wüst AP (2017) Diet, medication use and drug intake during pregnancy: data from the consecutive Swiss Health Surveys of 2007 and 2012. Swiss Med Wkly 147:w14572
Colbers A, Greupink R, Litjens C, Burger D, Russel FG (2016) Physiologically based modelling of darunavir/ritonavir pharmacokinetics during pregnancy. Clin Pharmacokinet 55:381–396
Dallmann A, Pfister M, van den Anker J, Eissing T (2018a) Physiologically based pharmacokinetic modeling in pregnancy: a systematic review of published models. Clin Pharmacol Ther 104:1110–1124
Dallmann A, van den Anker J, Pfister M, Koch G (2018b) Characterization of maternal and neonatal pharmacokinetic behavior of ceftazidime. J Clin Pharmacol 59:74–82
Etwel F, Hutson JR, Madadi P, Gareri J, Koren G (2014) Fetal and perinatal exposure to drugs and chemicals: novel biomarkers of risk. Annu Rev Pharmacol Toxicol 54:295–315
Evers KS et al (2018) Neurofilament as neuronal injury blood marker in preeclampsia. Hypertension 117:10314
Hartmanshenn C, Scherholz M, Androulakis IP (2016) Physiologically-based pharmacokinetic models: approaches for enabling personalized medicine. J Pharmacokinet Pharmacodyn 43:481–504. https://doi.org/10.1007/s10928-016-9492-y
Hines RN (2008) The ontogeny of drug metabolism enzymes and implications for adverse drug events. Pharmacol Ther 118:250–267
Huppertz B (2018) An updated view on the origin and use of angiogenic biomarkers for preeclampsia. Expert Rev Mol Diagn:1–9. https://doi.org/10.1080/14737159.2018.1546579
Karumanchi SA (2016) Angiogenic factors in preeclampsia: from diagnosis to therapy. Hypertension 67:1072–1079. https://doi.org/10.1161/HYPERTENSIONAHA.116.06421
Kastl JT (2017) Renal function in the fetus and neonate–the creatinine enigma. In: Seminars in fetal and neonatal medicine, vol 2. Elsevier, Amsterdam, pp 83–89
Ke AB, Greupink R, Abduljalil K (2018) Drug dosing in pregnant women: challenges and opportunities in using physiologically based pharmacokinetic modeling and simulations. CPT Pharmacometrics Syst Pharmacol 7:103–110
Kearns GL, Abdel-Rahman SM, Alander SW, Blowey DL, Leeder JS, Kauffman RE (2003) Developmental pharmacology—drug disposition, action, and therapy in infants and children. N Engl J Med 349:1157–1167
Kesho Bora Study Group (2011) Triple antiretroviral compared with zidovudine and single-dose nevirapine prophylaxis during pregnancy and breastfeeding for prevention of mother-to-child transmission of HIV-1 (Kesho Bora study): a randomised controlled trial. Lancet Infect Dis 11:171–180
Koch G, Datta AN, Jost K, Schulzke SM, van den Anker J, Pfister M (2017) Caffeine citrate dosing adjustments to assure stable caffeine concentrations in preterm neonates. J Pediatr 191:50–56.e51
Koren G (1997) Therapeutic drug monitoring principles in the neonate. Clin Chem 43:222–227
Koren G, Hutson J, Gareri J (2008) Novel methods for the detection of drug and alcohol exposure during pregnancy: implications for maternal and child health. Clin Pharmacol Ther 83:631–634
Ku LC, Smith PB (2014) Dosing in neonates: special considerations in physiology and trial design. Pediatr Res 77:2
Kumer K, Premru-Srsen T, Fabjan-Vodusek V, Tul N, Fabjan T, Osredkar J (2018) Peripheral arterial tonometry and angiogenic biomarkers in preeclampsia. Hypertens Pregnancy 37:197–203. https://doi.org/10.1080/10641955.2018.1524478
Levine RJ et al (2004) Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 350:672–683. https://doi.org/10.1056/NEJMoa031884
Loebstein R, Lalkin A, Koren G (1997) Pharmacokinetic changes during pregnancy and their clinical relevance. Clin Pharmacokinet 33:328–343
Manokhina I, Del Gobbo GF, Konwar C, Wilson SL, Robinson WP (2017) Review: placental biomarkers for assessing fetal health. Hum Mol Genet 26:R237–R245
Manolis E, Pons G (2009) Proposals for model-based paediatric medicinal development within the current European Union regulatory framework. Br J Clin Pharmacol 68:493–501
Mayeux R (2004) Biomarkers: potential uses and limitations. NeuroRx 1:182–188
Maynard SE, Karumanchi SA (2011) Angiogenic factors and preeclampsia. Semin Nephrol 31:33–46. https://doi.org/10.1016/j.semnephrol.2010.10.004
Mitchell AA, Gilboa SM, Werler MM, Kelley KE, Louik C, Hernández-Díaz S, Study NBDP (2011) Medication use during pregnancy, with particular focus on prescription drugs: 1976-2008. Am J Obstet Gynecol 205:51. e51–51. e58
Moore TJ, Weiss SR, Kaplan S, Blaisdell CJ (2002) Reported adverse drug events in infants and children under 2 years of age. Pediatrics 110:e53–e53
Morton SU, Brodsky D (2016) Fetal physiology and the transition to extrauterine life. Clin Perinatol 43:395–407
Pariente G, Leibson T, Carls A, Adams-Webber T, Ito S, Koren G (2016) Pregnancy-associated changes in pharmacokinetics: a systematic review. PLoS Med 13:e1002160
Risch M et al (2017) High first-trimester maternal blood cystatin C levels despite normal serum creatinine predict pre-eclampsia in singleton pregnancies. Scand J Clin Lab Invest 77:634–643. https://doi.org/10.1080/00365513.2017.1393692
Saint-Faust M, Boubred F, Simeoni U (2014) Renal development and neonatal adaptation. Am J Perinatol 31:773–780
Schalkwijk S, Buaben AO, Freriksen JJ, Colbers AP, Burger DM, Greupink R, Russel FG (2018) Prediction of fetal darunavir exposure by integrating human ex-vivo placental transfer and physiologically based pharmacokinetic modeling. Clin Pharmacokinet 57:705–716
Seyberth HW, Kauffman RE (2011) Basics and dynamics of neonatal and pediatric pharmacology. In: Pediatric clinical pharmacology. Springer, Berlin, pp 3–49
Steegers EA, Von Dadelszen P, Duvekot JJ, Pijnenborg R (2010) Pre-eclampsia. Lancet 376:631–644
Stout SA, Espel EV, Sandman CA, Glynn LM, Davis EP (2015) Fetal programming of children’s obesity risk. Psychoneuroendocrinology 53:29–39
Sulemanji M, Vakili K (2013) Neonatal renal physiology. In: Seminars in pediatric surgery, vol 4. Elsevier, Amsterdam, pp 195–198
van den Anker J, Reed MD, Allegaert K, Kearns GL (2018) Developmental changes in pharmacokinetics and pharmacodynamics. J Clin Pharmacol 58:S10–S25
van Donge T, Pfister M, Bielicki J, Csajka C, Rodieux F, van den Anker J, Fuchs A (2018) Quantitative analysis of gentamicin exposure in neonates and infants calls into question its current dosing recommendations. Antimicrob Agents Chemother 62:02004–02017
Venkatesha S et al (2006) Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med 12:642–649. https://doi.org/10.1038/nm1429
Widmer M et al (2015) Accuracy of angiogenic biomarkers at ≤20 weeks’ gestation in predicting the risk of pre-eclampsia: a WHO multicentre study. Pregnancy Hypertens 5:330–338
Wilbaux M, Kasser S, Wellmann S, Lapaire O, Van Den Anker JN, Pfister M (2016) Characterizing and forecasting individual weight changes in term neonates. J Pediatr 173:101–107. e110
Zhang Z, Unadkat JD (2017) Development of a novel maternal-fetal physiologically based pharmacokinetic model II: verification of the model for passive placental permeability drugs. Drug Metab Dispos 45:939–946
Zhang Z, Imperial MZ, Patilea-Vrana GI, Wedagedera J, Gaohua L, Unadkat JD (2017) Development of a novel maternal-fetal physiologically based pharmacokinetic model I: insights into factors that determine fetal drug exposure through simulations and sensitivity analyses. Drug Metab Dispos 45:920–938
Acknowledgment
TvD, KE, GK, JvdA, and MP would like to thank the Eckenstein-Geigy Foundation in Basel, Switzerland, for their financial support.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
van Donge, T., Evers, K., Koch, G., van den Anker, J., Pfister, M. (2019). Clinical Pharmacology and Pharmacometrics to Better Understand Physiological Changes During Pregnancy and Neonatal Life. In: Kiess, W., Schwab, M., van den Anker, J. (eds) Pediatric Pharmacotherapy . Handbook of Experimental Pharmacology, vol 261. Springer, Cham. https://doi.org/10.1007/164_2019_210
Download citation
DOI: https://doi.org/10.1007/164_2019_210
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-50493-9
Online ISBN: 978-3-030-50494-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)