Abstract
Overfeeding of fat can cause various metabolic disorders including obesity and type 2 diabetes (T2D). Diet provided free fatty acids (FFAs) are not only essential nutrients, but they are also recognized as signaling molecules, which stimulate various important biological functions. Recently, several G protein-coupled receptors (GPCRs), including FFA1-4, have been identified as receptors of FFAs by various physiological and pharmacological studies. FFAs exert physiological functions through these FFA receptors (FFARs) depending on carbon chain length and degree of unsaturation. Functional analyses have revealed that several important metabolic processes, such as peptide hormone secretion, cell maturation and nerve activities, are regulated by FFARs and thereby FFARs contribute to the energy homeostasis through these physiological functions. Hence, FFARs are expected to be promising pharmacological targets for metabolic disorders since imbalances in energy homeostasis lead to metabolic disorders. In human, it is established that different responses of individuals to endogenous ligands and chemical drugs may be due to differences in the ability of such ligands to activate nucleotide polymorphic variants of receptors. However, the clear links between genetic variations that are involved in metabolic disorders and polymorphisms receptors have been relatively difficult to assess. In this review, I summarize current literature describing physiological functions of FFARs and genetic variations of those receptors to discuss the potential of FFARs as drug targets for metabolic disorders.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Diabetes
- Energy homeostasis
- FFARs
- Free fatty acids
- Genetic variations
- Genetics
- Glucose
- GPCRs
- Insulin
- Mutation
- Polymorphic variations
- Polymorphism
- SNPs
1 Introduction
A lot of recent studies have revealed that various biomolecules derived from dietary foods, such as carbohydrate, lipid, and fiber, previously considered simply as nutrients and components of the body also act as essential signaling molecules to sense metabolic state and regulate whole body energy metabolism through, at least in part, members of the family of G protein-coupled receptors (GPCRs) (Priyadarshini et al. 2016; Watterson et al. 2014; Ulven and Christiansen 2015). Hence, from these aspects, dietary components have been considered as hormones (Ryan and Seeley 2013). Nutritional status is transmitted by the catabolites of food, which provides various simple biomolecules including free fatty acids (FFAs) in order to form a feedback loop. For example, short-chain fatty acids (SCFAs), which are generated by intestinal microbiota through fermentation of dietary fiber in the gut, not only act directly in the gut in which they are generated, but also stimulate various cell types such as immune cells and adipocytes after transport throughout the systemic circulation. Because of these characteristics, SCFAs are defined as hormone like biomolecules (Kimura et al. 2013; Maslowski et al. 2009; Macia et al. 2015; Masui et al. 2013; Trompette et al. 2014). Generally, mammals use not only glucose but also FFAs as key energy sources (Offermanns 2014; Spector and Kim 2014). On the other hand, a number of recent studies revealed that FFAs also act as signaling molecules to regulate a lot of physiological functions via their corresponding receptors. Several GPCRs have been successfully identified as receptors of FFAs (Brown et al. 2003; Briscoe et al. 2003; Itoh et al. 2003; Kotarsky et al. 2003a; Le Poul et al. 2003; Nilsson et al. 2003). SCFAs activate FFA2 and FFA3 whilst medium-chain and long-chain FFAs (MCFAs/LCFAs) activate FFA1 and FFA4 (Hirasawa et al. 2005; Itoh et al. 2003; Steneberg et al. 2005). FFAs regulate energy homeostasis via activation of these various FFAs receptors (FFARs) (Sekiguchi et al. 2015; Oh et al. 2010; Kimura et al. 2011; Ichimura et al. 2012; Oh and Olefsky 2012; Kimura et al. 2013). FFARs are expressed in various tissues and cell types. Therefore, these receptors mediate essential physiological and pathological functions of FFAs in these tissues and cells. Hence, FFARs have potential as therapeutic targets of diseases, in particular metabolic disorders.
The genetic variation in the sequence of the same GPCR, resulting from non-synonymous single nucleotide polymorphisms (SNPs), can result in substantial differences in pharmacology and function of the receptor (Balasubramanian et al. 2005; Taneera et al. 2012). However, the functional changes and capacity of enzymes involved in drug metabolism are routinely considered as the main challenges of stratified medicine and individual use of therapeutics (Zhou et al. 2009). Recent genome-wide association studies showed that GPCRs including FFARs are also linked to disease via such SNPs (Insel et al. 2007; Taneera et al. 2012). Hence, in this review, I summarize and discuss the recent advances in research regarding FFARs and their polymorphisms.
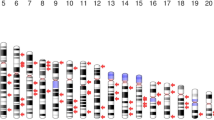
2 Free Fatty Acid Receptors
More than 800 GPCRs are encoded in the human genomic DNA. Among them, approximately 350 GPCRs have been demonstrated to be activated by endogenously produced ligands (Fredriksson et al. 2003). The development of synthetic agonists and antagonists of specific GPCRs is essential to understand the physiological and pathological functions of individual receptors, as GPCRs have essential roles in the regulation of major physiological and pathological responses. Among the numbers of GPCRs which are stimulated and activated by metabolic biomolecules at least four receptors are identified as FFARs (Stoddart et al. 2008b). The GPR40 family genes, including GPR40, GPR41, GPR42, and GPR43 were identified in the course of a search for novel human galanin receptor subtypes in 1997 (Sawzdargo et al. 1997). The efforts to deorphanize these receptors successfully revealed that of these receptors, GPR40, GPR41 and GPR43 were activated by FFAs (Briscoe et al. 2003; Brown et al. 2003; Kotarsky et al. 2003a, b; Le Poul et al. 2003; Nilsson et al. 2003), and therefor these receptors were recognized as FFARs. They were renamed as FFA1, FFA3, and FFA2, respectively. GPR42 was first reported as inactive and a potential pseudogene. However, GPR42 was recently reported to be a functional polymorphism of GPR41. Overall identity between sequences of GPR42 and GPR41 is 98%. Furthermore, the transmembrane domain regions of GPR42 are 100% identical to that of GPR41 (Liaw and Connolly 2009). Subsequently, the phylogenetically distinct receptor for FFAs, GPR120, which was also renamed as FFA4 was identified (Hirasawa et al. 2005). FFA1, FFA2, and FFA3 genes are encoded closely at chromosome 19q13.1 and form a highly related gene family group in human (Stoddart et al. 2008b). Hence, these genes presumably developed from a single common ancestor via gene duplication. In contrast, FFA4 is not closely related in sequence to the other FFARs despite being activated by an overlapping group of MCFAs and LCFAs as FFA1 (Ichimura et al. 2014; Hirasawa et al. 2005). In addition to the current FFA family members, there are several additional GPCRs, which appear to be activated by FFAs. GPR84 is an orphan receptor that recognizes MCFAs (Nagasaki et al. 2012; Suzuki et al. 2013), while the mouse olfactory receptor Olf78 (OR51E2 in human) appears to be activated by the SCFAs (Pluznick et al. 2013; Pluznick 2014). The following sections of this review will summarize recent advances in research regarding FFARs and their polymorphisms.
3 Polymorphic Variation of Receptors for SCFAs
SCFAs consist of carbon chain length from C2 to C6 and have various roles in physiological and pathological conditions. Generally, mammals use glucose as the main metabolic fuel under normal feeding conditions. SCFAs are produced by gut microbial fermentation of indigestible polysaccharides, including dietary fiber. Intestinal microbiota-derived SCFAs contribute a significant proportion of the daily energy requirement (Bergman 1990; Flint et al. 2008). On the other hand, the identification and deorphanization of FFA2 and FFA3 resulted in SCFAs being considered as signaling molecules through these receptors (Brown et al. 2003; Briscoe et al. 2003; Le Poul et al. 2003). FFA2 and FFA3 share 38% sequence identity with selectivity toward different fatty acid carbon chain length. Signaling through these receptors mediates numerous effects. Early studies identified various immune cells as expressing both of the SCFA receptors. In particular, FFA2 is highly expressed in monocytes and polymorphonuclear cells (Brown et al. 2003; Le Poul et al. 2003; Nilsson et al. 2003). Both FFA2 and FFA3 are expressed in the gut, primarily by various enteroendocrine cells (Karaki et al. 2006, 2008; Tazoe et al. 2008, 2009). This may not be surprising, since the SCFAs are generated primarily in the gut through fermentation of dietary fiber. Both FFA2 and FFA3 have also been reported to be expressed in pancreatic β-cells (Kebede et al. 2008). Currently, the role of these receptors in regulating insulin secretion are attracting increasing attention (McNelis et al. 2015; Priyadarshini and Layden 2015; Priyadarshini et al. 2015; Tang et al. 2015). Expression of both FFA2 and FFA3 in adipose tissue has also been reported (Xiong et al. 2004; Han et al. 2014). Although the expression of FFA3 has been controversial, many studies have reported only FFA2 expression in adipose tissue (Hong et al. 2005; Hudson et al. 2013a; Zaibi et al. 2010). Many reports have revealed that FFA3 is expressed in the neurons present in both sympathetic ganglia and the enteric nervous system (Inoue et al. 2012; Kimura et al. 2011; Nohr et al. 2015). Furthermore, expression of both FFA2 and FFA3 has been found in various cancers, including breast, colon and liver cancer (Bindels et al. 2012; Tang et al. 2011; Yonezawa et al. 2007). Given these important roles of FFA2 and FFA3, genetic variation of these receptors could have various physiological and pathological effects.
3.1 FFA3 Functions and Polymorphisms
The deorphanization of FFA3 was reported in 2003. FFA3 was identified as a receptor for SCFAs (Brown et al. 2003; Le Poul et al. 2003). FFA3 is activated by SCFAs such as propionate (C3), butyrate (C4), and valerate (C5), which are produced by gut microbial fermentation of dietary fiber, with a rank order potency of C3 = C4 = C5 > C6 > C2 > C1 (Brown et al. 2003; Le Poul et al. 2003). Although FFA3 and FFA2 share the same SCFAs as ligands, the activation of FFA3 stimulates signaling pathways distinct from those of FFA2. FFA2 couples to both Gi/o and Gq pathways, but FFA3 couples only to Gi/o signaling (Stoddart et al. 2008b). Hence, ligand stimulation of FFA3 activates intracellular calcium ([Ca2+]i) responses and the phosphorylation of ERK1/2, but inhibits cAMP production. FFA3 is reported to be expressed in adipose tissue, intestinal tract, and the peripheral nervous system (Brown et al. 2003; Le Poul et al. 2003; Samuel et al. 2008; Kimura et al. 2011). Early FFA3 studies reported that FFA3 is highly expressed in adipose tissue and in adipocyte cell lines (Brown et al. 2003). FFA3 was reported to stimulate the secretion of leptin from adipocytes (Xiong et al. 2004). FFA3 knockdown decreased leptin secretion, whereas overexpression of FFA3 increased it (Xiong et al. 2004). Furthermore, propionate-stimulated leptin secretion was inhibited by pretreatment with pertussis toxin, which inhibits Gi/o G proteins (Al-Lahham et al. 2010). However, these reports have been controversial because of many conflicting reports as to whether FFA3 and/or FFA2 is expressed in adipose tissue and adipocytes (Hong et al. 2005; Bellahcene et al. 2013; Zaibi et al. 2010). Many other groups failed to detect mRNA and/or protein expression of FFA3 in mouse adipose tissue (Kimura et al. 2011, 2013; Hong et al. 2005). In contrast, FFA2 expression has clearly been detected in mouse adipose tissues. Our study using FFA2-KO mice demonstrated that blood leptin levels were not affected by deficiency of FFA2, however, they were decreased by adipocyte-specific overexpression of FFA2 (Kimura et al. 2013). Since the effect of SCFAs on leptin secretion was eliminated by pertussis toxin treatment, this indicates that SCFA-mediated leptin secretion is linked with Gi/o-mediated signaling pathways (Xiong et al. 2004). Hence, either FFA2 and/or FFA3 could be involved in leptin secretion. Our study demonstrated that in vivo C2 administration suppressed insulin signaling in adipocytes of wild-type but not FFA2-KO mice (Kimura et al. 2013). By using adipocytes from FFA2-KO mice, it was clearly demonstrated that C2 inhibited insulin-stimulated glucose uptake in wild-type but not FFA2-KO mice and that this was blocked by pertussis toxin treatment but not by a Gq-targeted siRNA (Kimura et al. 2013). Hence, SCFA-stimulated leptin secretion appears to be mediated via FFA2, not FFA3 (Kimura et al. 2013). However, FFA3 knockdown or knockout can be associated with concomitant down-regulation of FFA2 expression (Zaibi et al. 2010). These controversial results made data interpretation difficult (Hudson et al. 2013b). Our recent studies have revealed functional roles of FFA3 expressed in the sympathetic ganglion in controlling energy expenditure in both fed and fasting states (Kimura et al. 2011). Adult FFA3-KO mice showed reduced noradrenaline. In addition, heart rate of FFA3-KO mice was decreased. Propionate increased energy expenditure and heart rate in adult WT mice, whereas these effects were abolished in FFA3-KO mice. Moreover, the effect of propionate on the heart rate was suppressed by pretreatment with a β-adrenergic receptor blocker. These observations suggested that propionate activated the sympathetic nervous system via FFA3 (Kimura et al. 2013). Our study further demonstrated that FFA3 mediates propionate-stimulated release of noradrenaline from sympathetic neurons (Inoue et al. 2012; Kimura et al. 2013). In addition, β-hydroxybutyrate (β-HB) inhibited FFA3 activity (Kimura et al. 2013). β-HB, which is biosynthesized in liver under low-carbohydrate fed conditions, suppressed propionate-induced sympathetic activation in both primary cultured sympathetic neurons and intact mice (Inoue et al. 2012; Kimura et al. 2013). These findings indicate that biological functions of FFA3, such as sympathetic nervous system (SNS) activation by propionate and SNS inhibition by ketone bodies, might be involved in recognition of the energy condition in the body and thereby contribute to the maintenance of energy homeostasis. FFA3 is reported to be expressed in pancreatic β-cells, certain insulin-producing β-cell lines, such as MIN6, NIT-1, and βTC-6 and several types of cells in the gut (Samuel et al. 2008; Tazoe et al. 2008, 2009; Kebede et al. 2009; Zaibi et al. 2010). For example, FFA3 is expressed in peptide YY (PYY) containing enteroendocrine L cells (Tazoe et al. 2009). Samuel et al. showed that glucagon-like peptide (GLP-1) and PYY secretion is reduced in FFA3-KO mice. Tolhurst et al. reported that both C2 and C3 stimulated GLP-1 release from primary murine colonic cultures and that this was not blocked by treatment of the cells with pertussis toxin, indicating a non-Gi/o-mediated pathway. This effect was lost in cultures derived from FFA2-KO but not FFA3-KO mice. Since C2 and C3 increased [Ca2+]i, it was concluded that the SCFAs increased GLP-1 via a FFA2-Gq/11-mediated pathway (Tolhurst et al. 2012). Recently, Psichas et al. demonstrated that intracolonic infusion of C3 increased secretion of both GLP-1 and PYY in vivo and that these effects were abolished in FFA2-KO mice. Hence, these studies confirmed that SCFAs stimulate gut hormone secretion via FFA2 in vivo. In addition to enteroendocrine cells, FFA2 and FFA3 are also expressed in the stomach, and in particular, these receptors appear to be expressed in ghrelin-containing cells (Engelstoft et al. 2015). Hence, both C2 and C3 appear to inhibit ghrelin secretion.
SCFAs are produced in the colon through bacterial fermentation of mainly dietary fiber. Many studies have established strong links between the gut microbiota, health, and disease (Ley et al. 2006; Karlsson et al. 2013; Flint et al. 2012, 2015). Hence, many studies have aimed to assess whether FFA2 and/or FFA3 utilise bacterial microbial fermentation produced SCFAs in order to demonstrate links between the gut microbiota and health. Samuel et al. found that conventionally raised FFA3-KO mice had decreased adiposity compared to wild-type controls, but this was not apparent in germ-free (GF) mice (Samuel et al. 2008). In particular, this appeared to relate to PYY levels, which were decreased in FFA3-KO mice when gut microbiota were present but were not in GF mice. One study has also linked dietary fiber, the microbiota, SCFAs, and FFA3 to allergic airway disease (Trompette et al. 2014). In the study, a high-fiber diet altered microbiota composition in both the gut and the lung, increasing SCFA levels, and protected against allergic airway disease. Exogenous C3 administration was found to produce similar effects to fiber, but such effects of C3 were absent in FFA3-KO but not FFA2-KO mice.
Sawzdargo et al. showed that GPR42 is encoded in tandem with FFA1, FFA2, and FFA3 on human chromosome 19q13.1 (Sawzdargo et al. 1997). GPR42 is considered to be generated by tandem duplication of FFA3 (GPR41). FFA3 and GPR42 share 98% sequence identity. The differences are only in six amino acid positions (Fig. 1). Mutation of FFA3 residue 174th Arg to Trp, which is found in 174th position of GPR42, makes FFA3 non-responsive to SCFAs. Conversely, the reciprocal mutation in GPR42 restored partial functional responsiveness. Hence, GPR42 was firstly reported as an inactive, potential pseudogene (Brown et al. 2003). However, the six amino acid differences between FFA3 and GPR42 are currently considered as polymorphic variants (Liaw and Connolly 2009). The functional Arg174 allele was detected in 61% of those subjects at the GPR42 locus based on a genotyping study of the corresponding alleles from a population of more than 100 subjects (Liaw and Connolly 2009). Recently, Puhl et al. sequenced the open reading frames of FFA3 and GPR42 from 56 individuals and found a high frequency of polymorphisms, contributing to several complex haplotypes (Puhl et al. 2015). They also identified a structural variation that results in GPR42 copy number polymorphism with a frequency of 18.8%. Sequencing analysis further demonstrated that 50.6% of GPR42 haplotypes differed from FFA3 by only a single non-synonymous substitution and that the GPR42 reference sequence matched only 4.4% of the alleles. These data suggested that GPR42 should be reclassified as a functional gene, and thereby copy number polymorphism of FFA3/GPR42 might be considered during genetic and pharmacological investigation of these receptors. Techniques for determining mRNA expression, such as Northern blot analysis, TaqMan, and RT-PCR, would be unable to distinguish FFA3 mRNA from GPR42 mRNA. Hence, previously reported FFA3 mRNA expression profiles are likely to includ both FFA3 and GPR42 expression.
169 variants of FFA3 are listed in a genetic variation database based on the 1000 genomes project (Genomes Project et al. 2015). 45th position of the amino acid sequence is one of the non-consensus residues between FFA3 and GPR42. The most common genetic variant reported is Arg45His (MAF score of 18.5%). the original FFA3/GPR42 genetic study also reported the His45 minor allele of FFA3 in one subject (Liaw and Connolly 2009). However, interchange with the GPR42 allele in 45th position, Arg45Cys, did not affect FFA3 function (Brown et al. 2003). Therefore, this position may have relatively little effect on receptor function. On the other hand, Asp158Asn and Arg185Gln, which are rarely described as missense variants, would be expected to have significant effects on FFA3 function. Hudson et al. have previously reported that FFA3 residue Asp158 is involved in forming an ionic lock interaction between arginine residues in the SCFA binding pocket that limit ligand-independent activation of the receptor (Hudson et al. 2012b). They also reported that the mouse orthologue, which displays marked constitutive activity, has an Asn residue at this position. Hence, humans carrying the Asp158Asn allele would yield an increased constitutively active FFA3 that may be relatively sensitive to endogenous ligands. Arg185 of FFA3 is conserved between FFA1 and FFA3. This residue is critical for ligand recognition and anchoring of the carboxylate moiety of the SCFAs to the binding pocket (Sum et al. 2007; Stoddart et al. 2008a). The mutation at this position has been reported to abolish SCFA interactions. Hence, Arg185Gln variant carriers are likely to be nonresponsive to SCFAs.
3.2 FFA2 Functions and Polymorphisms
FFA2 was reported to be activated by acetate (C2) through ligand screening studies for bioactive compounds by using [Ca2+]i analyses (Brown et al. 2003; Nilsson et al. 2003). Although both FFA2 and FFA3 are activated by SCFAs, potency of the SCFAs for these receptors is clearly different (Brown et al. 2003; Hudson et al. 2012a). Previous structure-activity relationship studies demonstrated that FFA2 exhibited a preference for smaller SCFAs compared to FFR3. FFR2 is activated by high micromolar or millimolar concentrations of SCFAs, such as propionate (C3), butyrate (C4) and substantially less so by caproate (C6) and formate (C1) with a rank order potency of C2 = C3 > C4 > C6 > C5 > C1 (Brown et al. 2003; Le Poul et al. 2003). As described above, FFA2 couples to both pertussis toxin-sensitive Gi/o and Gq pathways (Andoh et al. 2003; Le Poul et al. 2003). The activation of FFA2 by endogenous agonists not only inhibits cAMP production through interactions with Gi/o G proteins but also causes [Ca2+]i elevation and promotes activation of the mitogen-activated protein kinase (MAPK) cascade via interactions with Gq family G proteins. FFA2 is expressed in immune cells, including neutrophils, monocytes and polymorphonuclear cells (Brown et al. 2003). In these cell types, FFA2 has an important role in immune cell recruitment in inflammatory responses (Le Poul et al. 2003; Sina et al. 2009; Maslowski et al. 2009; Vinolo et al. 2011). FFA2-chemotactic response was inhibited by pertussis toxin treatment, indicating that this response is mediated via Gi/o (Sina et al. 2009). Moreover, Masui et al. reported that production of tumor necrosis factor alpha from mononuclear cells was suppressed by acetate and that the effect was inhibited by an anti-FFA2 antibody (Masui et al. 2013). Kim et al. demonstrated that SCFAs activate FFA2 and FFA3 on intestinal epithelial cells, leading to mitogen-activated protein kinase signaling and rapid production of chemokines and cytokines (Kim et al. 2013). FFA2 expression was also detected in adipose tissue, intestines, and islet cells of the pancreas (Hong et al. 2005; Regard et al. 2008; Maslowski et al. 2009). In the adipose tissue, FFA2 activation promotes adipogenesis by increasing lipid accumulation (Hong et al. 2005) and inhibiting lipolysis (Ge et al. 2008). In a series of in vitro and in vivo studies, we found that whole-body deficiency of FFA2 induced obesity in mice, whereas mice with adipose tissue-specific overexpression of FFA2 are lean under normal conditions (Kimura et al. 2013). However, one study has reported conflicting results with FFA2-KO mice. Bjursell et al. reported that FFA2-KO mice have reduced body fat mass, improved glucose control, and increased insulin sensitivity (Bjursell et al. 2011). In primary human adipocytes, an absence of relationship between FFA2 and adipocyte differentiation was found, unlike what was observed in mice (Dewulf et al. 2013). Furthermore, in an acute model of colitis, two separate studies have reported conflicting results with FFA2-KO mice. One group showed reduced (Maslowski et al. 2009) and another group showed heightened (Sina et al. 2009) inflammatory responses. In the intestines, FFA2 is associated with the regulation of appetite and insulin signaling. The intestine contributes to energy homeostasis not only by nutrient absorption but also the secretion of incretin hormones (Turton et al. 1996; Batterham et al. 2002; Chelikani et al. 2005; Koda et al. 2005). FFA2-expressing cells are co-localized with PYY-containing enteroendocrine L-cells of the rat gastrointestinal tract (Karaki et al. 2006). Furthermore, FFA2 expression in the enteroendocrine L cells mediates SCFA-induced GLP-1 release in vitro and in vivo (Tolhurst et al. 2012). FFA2 is also present in pancreatic islets, specifically the β-cells, although its role in β-cell function remains unclear (Kebede et al. 2009). Two studies have found that SCFAs activate FFA2 to enhance glucose stimulated insulin secretion (GSIS) from murine islets both in vivo and in vitro and that this occurs through a Gq/11 and phospholipase C mediated pathway (McNelis et al. 2015; Priyadarshini et al. 2015). Another study indicated that SCFAs inhibit GSIS through both FFA2 and FFA3 and that this occurs through a Gi/o-mediated pathway. In contrast, SCFAs have no effect on GSIS in human islets, despite the fact that SCFAs activated both Gq and Gi signaling (Priyadarshini et al. 2015).
As described above, many researchers have made efforts to assess whether FFA2 and/or FFA3 mediate the functions of bacterial microbial fermentation produced SCFAs. The studies on FFA2 have demonstrated relationships between this receptor, SCFAs produced by gut microbiota and inflammatory responses. Maslowski et al. demonstrated that FFA2-KO mice showed exacerbated or unresolving inflammation in models of colitis, arthritis and asthma, indicating that stimulation of FFA2 by SCFAs was necessary for the normal inflammatory responses (Maslowski et al. 2009). GF mice, which were devoid of bacteria and generate little or no SCFAs, showed a similar dysregulation of inflammatory responses. Smith et al. showed that SCFAs produced by gut microbiota-derived bacterial fermentation regulated the size and function of the colonic regulatory T cell (TRegs) pool and protect against colitis in a FFA2-dependent manner in mice (Smith et al. 2013). It was shown that GF conditions reduced the population of TRegs in the intestine and that SCFAs restored these populations. Smith et al. demonstrated that the effects of SCFAs on GF mice were lacking in FFA2-KO mice. These data indicated that FFA2 mediated biological functions of SCFAs from gut microbiota.
The 1000 genomes project database lists 169 FFA2 variants (Genomes Project et al. 2015). The most common verified variant is Leu211His with a MAF value of 3.6%. However, at the current stage, no group has reported any relationship between this polymorphism and physiological function of FFA2 or the association with any disease/clinical phenotype, although this change in amino acid residue could possibly have impact on receptor function. The Leu211His variation could have effects on G protein coupling because the position is located in the receptor’s third intracellular loop. Arg255Gln, which is a relatively rare missense variant of FFA2, also affects the receptor function (Hudson et al. 2013b). Arg residue at this position is a conserved polar residue at the upper face of transmembrane domain VII, which facilitate binding of SCFAs to the receptor. Hence, carriers of this minor allelic variant would be anticipated to be unresponsive to endogenous ligands.
4 Polymorphic Variation of Receptors for LCFAs
MCFAs and LCFAs are defined as 6–12 carbon-chain fatty acids and >12 carbon-chain fatty acids, respectively. MCFAs and LCFAs are generally considered as key energy sources for the whole body (Offermanns 2014). However, the identification of FFA1 and FFA4 as receptors for MCFAs and LCFAs showed that these FFAs also have important roles in signaling transduction as signaling molecules (Itoh et al. 2003; Hirasawa et al. 2005; Ichimura et al. 2014). These FFAs, which are endogenous ligands of FFA1 and FFA4, are supplied by both food intake and de novo biosynthesis. However, FFAs, which are so called essential fatty acids, containing more than two double bonds, such as linoleic acid and docosahexaenoic acid (DHA), are not obtained by biosynthesis in humans. Hence, these essential fatty acids have to be supplied within food. Recent studies clearly demonstrated that FFA1 and FFA4 contribute to maintenance of systemic energy homeostasis (Itoh et al. 2003; Oh et al. 2010; Ichimura et al. 2012; Hara et al. 2014; Hudson et al. 2013b; Ichimura et al. 2014). Hence, FFA1 and FFA4 are prospective therapeutic targets for metabolic diseases.
4.1 FFA1 Functions and Polymorphisms
FFA1 is expressed predominantly in insulin-producing pancreatic β-cells and enhances GSIS (Briscoe et al. 2003; Itoh et al. 2003; Kotarsky et al. 2003b; Latour et al. 2007). Because of these characteristics, great attention has been paid to FFA1 as a therapeutic target of metabolic diseases. Loss-of-functional analyses of FFA1 by using RNA interference, chemical compounds, or genetic deletion in mice consistently result in a significant decrease in FFA-induced GSIS (Itoh and Hinuma 2005; Salehi et al. 2005; Steneberg et al. 2005; Briscoe et al. 2006; Latour et al. 2007; Schnell et al. 2007; Kebede et al. 2008; Lan et al. 2008). Several studies have demonstrated that the FFA1-mediated effect on GSIS is mediated through Gq/11-phospholipase C and L-type Ca2+ pathways (Fujiwara et al. 2005; Latour et al. 2007), leading to phosphorylation of protein kinase D1 and filamentous actin remodeling (Ferdaoussi et al. 2012). Furthermore, FFA1 expression is also detected in enteroendocrine cells and FFA1 agonists have been reported to stimulate release of the incretin hormone GLP-1 and PYY from L cells (Edfalk et al. 2008), cholecystokinin (CCK) from I cells (Liou et al. 2011) and gastric inhibitory peptide (GIP) from K cells (Sykaras et al. 2012). Hence, FFA1 decreases blood glucose not only by direct stimulation of insulin secretion from pancreatic β-cells, but also by GLP-1-mediated indirect stimulation of insulin secretion (Luo et al. 2012). FFA1 expression has been also reported in taste buds and cells of the central nervous system (Ma et al. 2007; Edfalk et al. 2008; Hirasawa et al. 2008; Cartoni et al. 2010; Liou et al. 2011; Sykaras et al. 2012). Altogether, FFA1 plays important roles in regulation of systemic glucose homeostasis. Given the physiological roles of FFA1 in glucose homeostasis, FFA1 agonists are expected to be potential medicines for the treatment of type 2 diabetes (T2D). Many compounds have been reported as FFA1 agonists, and some of have entered clinical trials (Briscoe et al. 2006; Tsujihata et al. 2011; Takano et al. 2014; Defossa and Wagner 2014; Christiansen et al. 2011, 2013a, b). In particular, TAK-875 was developed as an orally available FFA1 partial agonist. A phase III clinical trial employed TAK-875 as a glucose regulating therapeutic agent. However, TAK-875 was removed from these trials due to potential liver toxicity (Ichimura et al. 2014). TAK-875 enhances GSIS and improves both postprandial and hyperglycemia with a low risk of hypoglycemia (Tsujihata et al. 2011; Defossa and Wagner 2014), whereas it has no effect on glucagon secretion or insulin resistance (Araki et al. 2012; Bailey 2012; Burant et al. 2012; Leifke et al. 2012; Naik et al. 2012; Mancini and Poitout 2013; Poitout and Lin 2013). TAK-875 is reported to be an ago-allosteric modulator of FFA1 (Yabuki et al. 2013). Collectively, FFA1 agonists show promise as novel medicines for the treatment for T2D. However, there are a many complicating factors, such as genetic polymorphisms of human FFA1, conflicting results from animal studies, and differential biological effects of FFA1 agonists between species. Hence, physiological and pharmacological studies of FFA1 by using animal models appear to be difficult to compare.
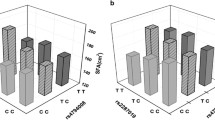
151 variants of human FFA1 were listed in the 1000 genomes project database (Genomes Project et al. 2015). Among them, Arg211His has been identified as a major variation of FFA1 with a MAF value of 18.2%. The effect of the Arg211His polymorphism in a Japanese male population was previously reported (Ogawa et al. 2005). Ogawa et al. demonstrated that individuals homozygous for the minor Arg variant displayed reduced serum insulin and β-cell function. These results suggested that the Arg211His polymorphism might contribute to insulin secretion via FFA1. On the other hand, Hamid et al. reported distinct results of this Arg211His polymorphism (Hamid et al. 2005). They employedd oral glucose tolerance tests and concluded that this polymorphism did not contribute to insulin secretion (Hamid et al. 2005). Moreover, no differences in allelic frequency between healthy and diabetic individuals have been found in either of these studies. No effect of Arg211His variation on FFA1 function has been detected by in vitro studies (Smith et al. 2009; Hamid et al. 2005). Hence this variant should be more carefully explored. Besides Arg211His polymorphism, some relatively rare variants of FFA1 have been assessed. MAF of Gly180Ser polymorphism is 0.42% in non-obese individuals. However, MAF of the variant is 1.07% in obese individuals and 2.60% in severely obese individuals (Vettor et al. 2008). Oral glucose tolerance testing of carriers of the polymorphism demonstrated that insulin secretion was significantly reduced in carriers of the minor Ser allele (Vettor et al. 2008). Furthermore, in vitro [Ca2+]i mobilization analysis indicated that the FFA1 variant reduced receptor function. However, Smith et al. failed to reproduce this in vitro result (Smith et al. 2009). Asp175Asn, which is another rare variation of FFA1, has also been reported to inhibit receptor function of FFA1 in vitro (Hamid et al. 2005). However, distinct results indicating that the receptor function of this variant is similar to the wild type have been also described (Smith et al. 2009). Since synthetic selective agonists have not been used on these variants, such analyses might be of considerable interest to examine. Not only missense polymorphisms, but also two kinds of SNPs upstream of the FFA1 gene associated with β-cell function has been reported (Kalis et al. 2007). The effect of three common SNPs of FFAR1 (rs2301151; rs16970264; rs1573611) on pancreatic function, body mass index (BMI), body composition and plasma lipids have been investigated. Although rs1573611 and rs2301151 were associated with some of these parameters, the authors concluded that differences in body composition and lipids associated with common SNPs in the FFA1 gene were apparently not mediated by changes in insulin sensitivity or β-cell function. Wagner et al. examined the interaction of genetic variation in FFA1 with FFAs and insulin secretion and revealed that the inverse association of FFAs and secretion of insulin was modulated by FFA1 SNP rs1573611 and became steeper for carriers of the minor allele (Wagner et al. 2013). Previously, it was reported that carriers of the minor allele of the Pro12Ala polymorphism (rs1805192) had lower insulin secretion during hyperglycemic clamp studies conducted with a concomitant intravenous lipid infusion, but no difference was seen between the genotypes without increasing blood FFAs (Stumvoll and Haring 2002). Based on this report, Wagner et al. demonstrated that two FFA1 SNPs (rs12462800 and rs10422744) were associated with reduced insulin secretion in participants concomitantly carrying a PPARγ minor allele and having high fasting FFAs (Wagner et al. 2014). These SNPs (rs12462800 and rs10422744) are located 0.8 kb apart in an intergenic regulatory area between the FFA1 and FFA3 genes, 3.5 and 3.8 kb from the 3′ end of the single FFA1 exon. These SNPs are more distal from the gene than the previously described FFA1 SNP rs1573611 which directly interacts with fasting FFAs in association with insulin secretion (Wagner et al. 2013). Collectively, although some kinds of studies established the relationships between polymorphisms of FFA1 and FFA1 receptor functions, further detailed analysis to elucidate the genetic variations, which effect FFA1 function or increase risk of metabolic diseases, is required.
4.2 FFA4 Functions and Polymorphisms
In 2005, FFA4 was deorphanized and identified as a FFA receptor (Hirasawa et al. 2005). FFA4 lacked substantial homology with GPR40 FFARs family members. Although the amino acid homology between FFA1 and FFA4 is only 10%, both of these receptors share similar endogenous ligands. FFA4 is activated by carbon-chain length 14–18 saturated FFAs C6 to C22 unsaturated FFAs (Fukunaga et al. 2006; Ichimura et al. 2014). Ligand stimulation of FFA4 increases [Ca2+]i but does not increase or decrease cAMP production in human or mouse FFA4-expresseing cells. Based on these and other results, FFA4 is coupled to Gq protein family (Hirasawa et al. 2005; Hara et al. 2009; Hudson et al. 2013c; Moore et al. 2009; Watson et al. 2012). FFA4-mediated increase of [Ca2+]i is blocked by the Gq/11-selective inhibitor YM-254890 (Hudson et al. 2013c). Recent studies indicated that some physiological function of FFA4 might be mediated by Gi-family G proteins. For example, pertussis toxin treatment blocked FFA4-mediated inhibition of ghrelin secretion from mouse gastric cells (Engelstoft et al. 2013) as well as somatostatin release from pancreatic islet delta cells (Stone et al. 2014). Stimulation of FFA4 also activates ERK1/2 and PI3-kinase signaling cascades (Katsuma et al. 2005; Hara et al. 2009). Furthermore, Oh et al. showed that stimulation of FFA4 by ω-3 FFAs contributes to anti-inflammatory responses (Oh et al. 2010). Such anti-inflammatory effects are exerted by the suppression of Toll-like receptor via a β-arrestin2 signaling pathway and transforming growth factor-β activated kinase 1 (TAK1) associated with TNF-α inflammation signaling pathway. FFA4 expression has also been detected in adipose tissue and adipocyte cell lines (Gotoh et al. 2007; Ichimura et al. 2012; Oh et al. 2010). In adipose tissue, FFA4 has been reported to contribute to adipocyte maturation (Gotoh et al. 2007; Ichimura et al. 2012) and glucose uptake through the induction of translocation of glucose transporter 4 (Oh et al. 2010). We have reported increased FFA4 expression in obese human subjects (Ichimura et al. 2012). On the other hand, there are conflicting results; Rodriguez-Pacheco et al. have reported decreased FFA4 expression in obese human subjects (Rodriguez-Pacheco et al. 2014). Although gene expression of FFA4 has been detected in pancreatic islet and cultured β-cell line, FFA4 does not appear to directly stimulate insulin secretion in pancreatic β-cells (Kebede et al. 2009; Taneera et al. 2012). Rather, FFA4 indirectly enhances insulin secretion by GLP-1 secretion from gut enteroendocrine cells (Hirasawa et al. 2005) and protects against cell death in pancreatic islet β-cells (Taneera et al. 2012). To date, limited reports indicated FFA4 expression in pancreatic α cells (Suckow et al. 2014) and δ cells (Stone et al. 2014). Moreover, FFA4 is also reported to be expressed in airway smooth muscle (Mizuta et al. 2015) and taste buds (Galindo et al. 2012; Matsumura et al. 2009). However, biological functions of FFA4 in these tissues are unclear or controversial (Martin et al. 2012; Ancel et al. 2015). FFA4 is expressed in the enteroendocrine cells on each of the L, K, and I cells (Hirasawa et al. 2005; Iwasaki et al. 2015; Sykaras et al. 2012). In addition, a direct correlation between BMI and FFA4 transcript levels have been observed in human duodenum (Little et al. 2014). Taken together, FFA4 is believed to be a potential therapeutic target for metabolic diseases, including T2D and obesity.
FFA4 was placed in the top 16 of the ranked list of the risk genes identified in whole genome studies to identify genes for T2D (Taneera et al. 2012). Furthermore, at least 18 missense polymorphisms of FFA4 have been listed in publically available databases (Genomes Project et al. 2015). Among these variants, the Arg67Cys polymorphism was identified as the only high frequency gene variation with a MAF value of 14.9% (Fig. 2). We have shown that this polymorphism has little effect however on pharmacological functions of FFA4 (Ichimura et al. 2012). Consistent with this result, the Arg67Cys variant has only a weak tendency toward an association between the polymorphism and obesity in humans with an odds ratio of 1.16. We have also identified the Arg270His polymorphism as a less common variant with a MAF value of 1.3–3%. We also showed that the Arg270His polymorphism is significantly associated with obesity with an odds ratio of 1.62 (Fig. 2). In vitro analyses successfully indicated that this polymorphism not only significantly reduced receptor function, but also acted as a dominant-negative like receptor. FFA4-KO mice fed a high-fat diet develop obesity, glucose intolerance and fatty liver with decreased adipocyte differentiation and lipogenesis and enhanced hepatic lipogenesis. These human and mice studies consistently showed that FFA4 has a key role in sensing dietary fat and, therefore, controlling energy balance. In addition to the gene polymorphisms, Moore et al. previously reported two splice variant isoforms of FFA4 (Moore et al. 2009). These splice variant isoforms are distinguished by the presence or absence of a 16-amino acid insertion, which is positioned in the third intracellular loop (Fig. 2). Studies of longer isoform function in mice or other rodents are not possible because the longer isoform of FFA4 exists only in human. Furthermore, the shorter isoform of FFA4 is coupled with both G protein-dependent and β-arrestin pathways, whereas the longer isoform is coupled only with the β-arrestin pathway (Watson et al. 2012). Additionally, the longer isoform of human FFA4 has been detected in only a few tissues, particularly in the colon (Galindo et al. 2012). Based on these reports, the function of human FFA4 may be at least to some extent different from FFA4 of other species. Hence, the functional and physiological importance of human long isoform remains uncertain. Recently, other groups also reported the relationship between this variant of FFA4 and human metabolism. Waguri et al. reported that genetic variation of FFA4 including this variant and dietary fat intake could be a possible determinant of BMI (Waguri et al. 2013). Bonnefond et al. also reported that this variant associated with increased fasting plasma glucose levels independent of BMI but not with measures of insulin resistance or T2D (Bonnefond et al. 2015). Furthermore, Marruzillo et al. reported that heterozygous child carriers of this FFA4 variant showed significantly higher alanine transaminase (ALT) levels than wild-type subjects, and also showed an odds ratio to have pathologic ALT (Marzuillo et al. 2014), indicating the relationship between liver injury in children and this variant. Recently, Vestmar et al. showed that this variant of FFA4 inhibited ligand-depending activation of Gq and Gi signalling in vitro (Vestmar et al. 2016). Since Vestmar et al. also used the shorter isoform for in vitro studies, these results also indicated that Arg254His variant reduced function in both Gq/11- and Gi/o-FFA4 signaling, although some function remained. Further, in this study, FFA4-arrestin interactions were not altered for this variant (Vestmar et al. 2016). Vestimar et al. failed to show the association of this variant with either increased risk of obesity or increased fasting plasma glucose levels in a Danish study population (Vestmar et al. 2016). It is not clear at present of the basis of these complicated results, however, as there is a very low frequency of this variant in the analyzed population, especially the age of subjects might affect the results. Our group, Waguri et al. and Bonnefond et al. included children, adolescent and adult individuals in the analyses. On the other hand, Vestmar et al. analyzed only adults. Based on these differences, further detailed analyses using more extreme cases or obesity among the young age subjects are needed to clarify the relationship between FFA4 variant and metabolic diseases.
5 Conclusions
FFAs, which are provided within the diet, via intestinal bacterial fermentation of dietary fiber, and de novo synthesis, act as important signaling molecules through FFARs. Hence, FFARs are seen as new potential therapeutic targets for metabolic disorders. To date, there is more attention on the effects of genetic variants of the FFARs on the pharmacology and functions of these receptors as these are one of causes of metabolic disorders. More detailed information of the relationship between genetic variations of FFARs and receptor function with selective ligands for each receptor might be required for the development of therapeutic agents targeting FFARs. A deeper understanding of the genetic variations of each member of FFAR family might open a new avenue of research in the development of therapeutic agents targeting FFARs.
References
Al-Lahham SH, Roelofsen H, Priebe M, Weening D, Dijkstra M, Hoek A, Rezaee F, Venema K, Vonk RJ (2010) Regulation of adipokine production in human adipose tissue by propionic acid. Eur J Clin Invest 40(5):401–407. doi:10.1111/j.1365-2362.2010.02278.x
Ancel D, Bernard A, Subramaniam S, Hirasawa A, Tsujimoto G, Hashimoto T, Passilly-Degrace P, Khan NA, Besnard P (2015) The oral lipid sensor GPR120 is not indispensable for the orosensory detection of dietary lipids in mice. J Lipid Res 56(2):369–378. doi:10.1194/jlr.M055202
Andoh A, Tsujikawa T, Fujiyama Y (2003) Role of dietary fiber and short-chain fatty acids in the colon. Curr Pharm Des 9(4):347–358
Araki T, Hirayama M, Hiroi S, Kaku K (2012) GPR40-induced insulin secretion by the novel agonist TAK-875: first clinical findings in patients with type 2 diabetes. Diabetes Obes Metab 14(3):271–278. doi:10.1111/j.1463-1326.2011.01525.x
Bailey CJ (2012) Could FFAR1 assist insulin secretion in type 2 diabetes? Lancet 379(9824):1370–1371. doi:10.1016/S0140-6736(12)60165-2
Balasubramanian S, Xia Y, Freinkman E, Gerstein M (2005) Sequence variation in G-protein-coupled receptors: analysis of single nucleotide polymorphisms. Nucleic Acids Res 33(5):1710–1721. doi:10.1093/nar/gki311
Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL, Wren AM, Brynes AE, Low MJ, Ghatei MA, Cone RD, Bloom SR (2002) Gut hormone PYY(3-36) physiologically inhibits food intake. Nature 418(6898):650–654. doi:10.1038/nature02666
Bellahcene M, O’Dowd JF, Wargent ET, Zaibi MS, Hislop DC, Ngala RA, Smith DM, Cawthorne MA, Stocker CJ, Arch JR (2013) Male mice that lack the G-protein-coupled receptor GPR41 have low energy expenditure and increased body fat content. Br J Nutr 109(10):1755–1764. doi:10.1017/S0007114512003923
Bergman EN (1990) Energy contributions of volatile fatty acids from the gastrointestinal tract in various species. Physiol Rev 70(2):567–590
Bindels LB, Porporato P, Dewulf EM, Verrax J, Neyrinck AM, Martin JC, Scott KP, Buc Calderon P, Feron O, Muccioli GG, Sonveaux P, Cani PD, Delzenne NM (2012) Gut microbiota-derived propionate reduces cancer cell proliferation in the liver. Br J Cancer 107(8):1337–1344. doi:10.1038/bjc.2012.409
Bjursell M, Admyre T, Goransson M, Marley AE, Smith DM, Oscarsson J, Bohlooly YM (2011) Improved glucose control and reduced body fat mass in free fatty acid receptor 2-deficient mice fed a high-fat diet. Am J Physiol Endocrinol Metab 300(1):E211–E220. doi:10.1152/ajpendo.00229.2010
Bonnefond A, Lamri A, Leloire A, Vaillant E, Roussel R, Levy-Marchal C, Weill J, Galan P, Hercberg S, Ragot S, Hadjadj S, Charpentier G, Balkau B, Marre M, Fumeron F, Froguel P (2015) Contribution of the low-frequency, loss-of-function p.R270H mutation in FFAR4 (GPR120) to increased fasting plasma glucose levels. J Med Genet 52(9):595–598. doi:10.1136/jmedgenet-2015-103065
Briscoe CP, Tadayyon M, Andrews JL, Benson WG, Chambers JK, Eilert MM, Ellis C, Elshourbagy NA, Goetz AS, Minnick DT, Murdock PR, Sauls HR Jr, Shabon U, Spinage LD, Strum JC, Szekeres PG, Tan KB, Way JM, Ignar DM, Wilson S, Muir AI (2003) The orphan G protein-coupled receptor GPR40 is activated by medium and long chain fatty acids. J Biol Chem 278(13):11303–11311. doi:10.1074/jbc.M211495200
Briscoe CP, Peat AJ, McKeown SC, Corbett DF, Goetz AS, Littleton TR, McCoy DC, Kenakin TP, Andrews JL, Ammala C, Fornwald JA, Ignar DM, Jenkinson S (2006) Pharmacological regulation of insulin secretion in MIN6 cells through the fatty acid receptor GPR40: identification of agonist and antagonist small molecules. Br J Pharmacol 148(5):619–628. doi:10.1038/sj.bjp.0706770
Brown AJ, Goldsworthy SM, Barnes AA, Eilert MM, Tcheang L, Daniels D, Muir AI, Wigglesworth MJ, Kinghorn I, Fraser NJ, Pike NB, Strum JC, Steplewski KM, Murdock PR, Holder JC, Marshall FH, Szekeres PG, Wilson S, Ignar DM, Foord SM, Wise A, Dowell SJ (2003) The Orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J Biol Chem 278(13):11312–11319. doi:10.1074/jbc.M211609200
Burant CF, Viswanathan P, Marcinak J, Cao C, Vakilynejad M, Xie B, Leifke E (2012) TAK-875 versus placebo or glimepiride in type 2 diabetes mellitus: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet 379(9824):1403–1411. doi:10.1016/S0140-6736(11)61879-5
Cartoni C, Yasumatsu K, Ohkuri T, Shigemura N, Yoshida R, Godinot N, le Coutre J, Ninomiya Y, Damak S (2010) Taste preference for fatty acids is mediated by GPR40 and GPR120. J Neurosci 30(25):8376–8382. doi:10.1523/JNEUROSCI.0496-10.2010
Chelikani PK, Haver AC, Reidelberger RD (2005) Intravenous infusion of peptide YY(3-36) potently inhibits food intake in rats. Endocrinology 146(2):879–888. doi:10.1210/en.2004-1138
Christiansen E, Urban C, Grundmann M, Due-Hansen ME, Hagesaether E, Schmidt J, Pardo L, Ullrich S, Kostenis E, Kassack M, Ulven T (2011) Identification of a potent and selective free fatty acid receptor 1 (FFA1/GPR40) agonist with favorable physicochemical and in vitro ADME properties. J Med Chem 54(19):6691–6703. doi:10.1021/jm2005699
Christiansen E, Due-Hansen ME, Urban C, Grundmann M, Schmidt J, Hansen SV, Hudson BD, Zaibi M, Markussen SB, Hagesaether E, Milligan G, Cawthorne MA, Kostenis E, Kassack MU, Ulven T (2013a) Discovery of a potent and selective free fatty acid receptor 1 agonist with low lipophilicity and high oral bioavailability. J Med Chem 56(3):982–992. doi:10.1021/jm301470a
Christiansen E, Hansen SV, Urban C, Hudson BD, Wargent ET, Grundmann M, Jenkins L, Zaibi M, Stocker CJ, Ullrich S, Kostenis E, Kassack MU, Milligan G, Cawthorne MA, Ulven T (2013b) Discovery of TUG-770: a highly potent free fatty acid receptor 1 (FFA1/GPR40) agonist for treatment of type 2 diabetes. ACS Med Chem Lett 4(5):441–445. doi:10.1021/ml4000673
Defossa E, Wagner M (2014) Recent developments in the discovery of FFA1 receptor agonists as novel oral treatment for type 2 diabetes mellitus. Bioorg Med Chem Lett 24(14):2991–3000. doi:10.1016/j.bmcl.2014.05.019
Dewulf EM, Ge Q, Bindels LB, Sohet FM, Cani PD, Brichard SM, Delzenne NM (2013) Evaluation of the relationship between GPR43 and adiposity in human. Nutr Metab 10(1):11. doi:10.1186/1743-7075-10-11
Edfalk S, Steneberg P, Edlund H (2008) Gpr40 is expressed in enteroendocrine cells and mediates free fatty acid stimulation of incretin secretion. Diabetes 57(9):2280–2287. doi:10.2337/db08-0307
Engelstoft MS, Park WM, Sakata I, Kristensen LV, Husted AS, Osborne-Lawrence S, Piper PK, Walker AK, Pedersen MH, Nohr MK, Pan J, Sinz CJ, Carrington PE, Akiyama TE, Jones RM, Tang C, Ahmed K, Offermanns S, Egerod KL, Zigman JM, Schwartz TW (2013) Seven transmembrane G protein-coupled receptor repertoire of gastric ghrelin cells. Mol Metab 2(4):376–392. doi:10.1016/j.molmet.2013.08.006
Engelstoft MS, Lund ML, Grunddal KV, Egerod KL, Osborne-Lawrence S, Poulsen SS, Zigman JM, Schwartz TW (2015) Research resource: a chromogranin a reporter for serotonin and histamine secreting enteroendocrine cells. Mol Endocrinol 29(11):1658–1671. doi:10.1210/me.2015-1106
Ferdaoussi M, Bergeron V, Zarrouki B, Kolic J, Cantley J, Fielitz J, Olson EN, Prentki M, Biden T, MacDonald PE, Poitout V (2012) G protein-coupled receptor (GPR)40-dependent potentiation of insulin secretion in mouse islets is mediated by protein kinase D1. Diabetologia 55(10):2682–2692. doi:10.1007/s00125-012-2650-x
Flint HJ, Bayer EA, Rincon MT, Lamed R, White BA (2008) Polysaccharide utilization by gut bacteria: potential for new insights from genomic analysis. Nat Rev Microbiol 6(2):121–131. doi:10.1038/nrmicro1817
Flint HJ, Scott KP, Louis P, Duncan SH (2012) The role of the gut microbiota in nutrition and health. Nat Rev Gastroenterol Hepatol 9(10):577–589. doi:10.1038/nrgastro.2012.156
Flint HJ, Duncan SH, Scott KP, Louis P (2015) Links between diet, gut microbiota composition and gut metabolism. Proc Nutr Soc 74(1):13–22. doi:10.1017/S0029665114001463
Fredriksson R, Lagerstrom MC, Lundin LG, Schioth HB (2003) The G-protein-coupled receptors in the human genome form five main families. Phylogenetic analysis, paralogon groups, and fingerprints. Mol Pharmacol 63(6):1256–1272. doi:10.1124/mol.63.6.1256
Fujiwara K, Maekawa F, Yada T (2005) Oleic acid interacts with GPR40 to induce Ca2+ signaling in rat islet beta-cells: mediation by PLC and L-type Ca2+ channel and link to insulin release. Am J Physiol Endocrinol Metab 289(4):E670–E677. doi:10.1152/ajpendo.00035.2005
Fukunaga S, Setoguchi S, Hirasawa A, Tsujimoto G (2006) Monitoring ligand-mediated internalization of G protein-coupled receptor as a novel pharmacological approach. Life Sci 80(1):17–23
Galindo MM, Voigt N, Stein J, van Lengerich J, Raguse JD, Hofmann T, Meyerhof W, Behrens M (2012) G protein-coupled receptors in human fat taste perception. Chem Senses 37(2):123–139. doi:10.1093/chemse/bjr069
Ge H, Li X, Weiszmann J, Wang P, Baribault H, Chen JL, Tian H, Li Y (2008) Activation of G protein-coupled receptor 43 in adipocytes leads to inhibition of lipolysis and suppression of plasma free fatty acids. Endocrinology 149(9):4519–4526. doi:10.1210/en.2008-0059
Genomes Project Consortium, Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, Marchini JL, McCarthy S, McVean GA, Abecasis GR (2015) A global reference for human genetic variation. Nature 526(7571):68–74. doi:10.1038/nature15393
Gotoh C, Hong YH, Iga T, Hishikawa D, Suzuki Y, Song SH, Choi KC, Adachi T, Hirasawa A, Tsujimoto G, Sasaki S, Roh SG (2007) The regulation of adipogenesis through GPR120. Biochem Biophys Res Commun 354(2):591–597
Hamid YH, Vissing H, Holst B, Urhammer SA, Pyke C, Hansen SK, Glumer C, Borch-Johnsen K, Jorgensen T, Schwartz TW, Pedersen O, Hansen T (2005) Studies of relationships between variation of the human G protein-coupled receptor 40 Gene and Type 2 diabetes and insulin release. Diabet Med 22(1):74–80. doi:10.1111/j.1464-5491.2005.01505.x
Han JH, Kim IS, Jung SH, Lee SG, Son HY, Myung CS (2014) The effects of propionate and valerate on insulin responsiveness for glucose uptake in 3T3-L1 adipocytes and C2C12 myotubes via G protein-coupled receptor 41. PLoS One 9(4):e95268. doi:10.1371/journal.pone.0095268
Hara T, Hirasawa A, Sun Q, Sadakane K, Itsubo C, Iga T, Adachi T, Koshimizu TA, Hashimoto T, Asakawa Y, Tsujimoto G (2009) Novel selective ligands for free fatty acid receptors GPR120 and GPR40. Naunyn Schmiedebergs Arch Pharmacol 380(3):247–255. doi:10.1007/s00210-009-0425-9
Hara T, Kashihara D, Ichimura A, Kimura I, Tsujimoto G, Hirasawa A (2014) Role of free fatty acid receptors in the regulation of energy metabolism. Biochim Biophys Acta 1841(9):1292–1300. doi:10.1016/j.bbalip.2014.06.002
Hirasawa A, Tsumaya K, Awaji T, Katsuma S, Adachi T, Yamada M, Sugimoto Y, Miyazaki S, Tsujimoto G (2005) Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat Med 11(1):90–94. doi:10.1038/nm1168
Hirasawa A, Hara T, Katsuma S, Adachi T, Tsujimoto G (2008) Free fatty acid receptors and drug discovery. Biol Pharm Bull 31(10):1847–1851
Hong YH, Nishimura Y, Hishikawa D, Tsuzuki H, Miyahara H, Gotoh C, Choi KC, Feng DD, Chen C, Lee HG, Katoh K, Roh SG, Sasaki S (2005) Acetate and propionate short chain fatty acids stimulate adipogenesis via GPCR43. Endocrinology 146(12):5092–5099. doi:10.1210/en.2005-0545
Hudson BD, Christiansen E, Tikhonova IG, Grundmann M, Kostenis E, Adams DR, Ulven T, Milligan G (2012a) Chemically engineering ligand selectivity at the free fatty acid receptor 2 based on pharmacological variation between species orthologs. FASEB J 26(12):4951–4965. doi:10.1096/fj.12-213314
Hudson BD, Tikhonova IG, Pandey SK, Ulven T, Milligan G (2012b) Extracellular ionic locks determine variation in constitutive activity and ligand potency between species orthologs of the free fatty acid receptors FFA2 and FFA3. J Biol Chem 287(49):41195–41209. doi:10.1074/jbc.M112.396259
Hudson BD, Due-Hansen ME, Christiansen E, Hansen AM, Mackenzie AE, Murdoch H, Pandey SK, Ward RJ, Marquez R, Tikhonova IG, Ulven T, Milligan G (2013a) Defining the molecular basis for the first potent and selective orthosteric agonists of the FFA2 free fatty acid receptor. J Biol Chem 288(24):17296–17312. doi:10.1074/jbc.M113.455337
Hudson BD, Murdoch H, Milligan G (2013b) Minireview: the effects of species ortholog and SNP variation on receptors for free fatty acids. Mol Endocrinol 27(8):1177–1187. doi:10.1210/me.2013-1085
Hudson BD, Shimpukade B, Mackenzie AE, Butcher AJ, Pediani JD, Christiansen E, Heathcote H, Tobin AB, Ulven T, Milligan G (2013c) The pharmacology of TUG-891, a potent and selective agonist of the free fatty acid receptor 4 (FFA4/GPR120), demonstrates both potential opportunity and possible challenges to therapeutic agonism. Mol Pharmacol 84(5):710–725. doi:10.1124/mol.113.087783
Ichimura A, Hirasawa A, Poulain-Godefroy O, Bonnefond A, Hara T, Yengo L, Kimura I, Leloire A, Liu N, Iida K, Choquet H, Besnard P, Lecoeur C, Vivequin S, Ayukawa K, Takeuchi M, Ozawa K, Tauber M, Maffeis C, Morandi A, Buzzetti R, Elliott P, Pouta A, Jarvelin MR, Korner A, Kiess W, Pigeyre M, Caiazzo R, Van Hul W, Van Gaal L, Horber F, Balkau B, Levy-Marchal C, Rouskas K, Kouvatsi A, Hebebrand J, Hinney A, Scherag A, Pattou F, Meyre D, Koshimizu TA, Wolowczuk I, Tsujimoto G, Froguel P (2012) Dysfunction of lipid sensor GPR120 leads to obesity in both mouse and human. Nature 483(7389):350–354. doi:10.1038/nature10798
Ichimura A, Hasegawa S, Kasubuchi M, Kimura I (2014) Free fatty acid receptors as therapeutic targets for the treatment of diabetes. Front Pharmacol 5:236. doi:10.3389/fphar.2014.00236
Inoue D, Kimura I, Wakabayashi M, Tsumoto H, Ozawa K, Hara T, Takei Y, Hirasawa A, Ishihama Y, Tsujimoto G (2012) Short-chain fatty acid receptor GPR41-mediated activation of sympathetic neurons involves synapsin 2b phosphorylation. FEBS Lett 586(10):1547–1554. doi:10.1016/j.febslet.2012.04.021
Insel PA, Tang CM, Hahntow I, Michel MC (2007) Impact of GPCRs in clinical medicine: monogenic diseases, genetic variants and drug targets. Biochim Biophys Acta 1768(4):994–1005. doi:10.1016/j.bbamem.2006.09.029
Itoh Y, Hinuma S (2005) GPR40, a free fatty acid receptor on pancreatic beta cells, regulates insulin secretion. Hepatol Res 33(2):171–173
Itoh Y, Kawamata Y, Harada M, Kobayashi M, Fujii R, Fukusumi S, Ogi K, Hosoya M, Tanaka Y, Uejima H, Tanaka H, Maruyama M, Satoh R, Okubo S, Kizawa H, Komatsu H, Matsumura F, Noguchi Y, Shinohara T, Hinuma S, Fujisawa Y, Fujino M (2003) Free fatty acids regulate insulin secretion from pancreatic beta cells through GPR40. Nature 422(6928):173–176. doi:10.1038/nature01478
Iwasaki K, Harada N, Sasaki K, Yamane S, Iida K, Suzuki K, Hamasaki A, Nasteska D, Shibue K, Joo E, Harada T, Hashimoto T, Asakawa Y, Hirasawa A, Inagaki N (2015) Free fatty acid receptor GPR120 is highly expressed in enteroendocrine K cells of the upper small intestine and has a critical role in GIP secretion after fat ingestion. Endocrinology 156(3):837–846. doi:10.1210/en.2014-1653
Kalis M, Leveen P, Lyssenko V, Almgren P, Groop L, Cilio CM (2007) Variants in the FFAR1 gene are associated with beta cell function. PLoS One 2(11):e1090. doi:10.1371/journal.pone.0001090
Karaki S, Mitsui R, Hayashi H, Kato I, Sugiya H, Iwanaga T, Furness JB, Kuwahara A (2006) Short-chain fatty acid receptor, GPR43, is expressed by enteroendocrine cells and mucosal mast cells in rat intestine. Cell Tissue Res 324(3):353–360. doi:10.1007/s00441-005-0140-x
Karaki S, Tazoe H, Hayashi H, Kashiwabara H, Tooyama K, Suzuki Y, Kuwahara A (2008) Expression of the short-chain fatty acid receptor, GPR43, in the human colon. J Mol Histol 39(2):135–142. doi:10.1007/s10735-007-9145-y
Karlsson F, Tremaroli V, Nielsen J, Backhed F (2013) Assessing the human gut microbiota in metabolic diseases. Diabetes 62(10):3341–3349. doi:10.2337/db13-0844
Katsuma S, Hatae N, Yano T, Ruike Y, Kimura M, Hirasawa A, Tsujimoto G (2005) Free fatty acids inhibit serum deprivation-induced apoptosis through GPR120 in a murine enteroendocrine cell line STC-1. J Biol Chem 280(20):19507–19515. doi:10.1074/jbc.M412385200
Kebede M, Alquier T, Latour MG, Semache M, Tremblay C, Poitout V (2008) The fatty acid receptor GPR40 plays a role in insulin secretion in vivo after high-fat feeding. Diabetes 57(9):2432–2437. doi:10.2337/db08-0553
Kebede MA, Alquier T, Latour MG, Poitout V (2009) Lipid receptors and islet function: therapeutic implications? Diabetes Obes Metab 11(Suppl 4):10–20. doi:10.1111/j.1463-1326.2009.01114.x
Kim MH, Kang SG, Park JH, Yanagisawa M, Kim CH (2013) Short-chain fatty acids activate GPR41 and GPR43 on intestinal epithelial cells to promote inflammatory responses in mice. Gastroenterology 145(2):396–406.e1–10. doi:10.1053/j.gastro.2013.04.056
Kimura I, Inoue D, Maeda T, Hara T, Ichimura A, Miyauchi S, Kobayashi M, Hirasawa A, Tsujimoto G (2011) Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein-coupled receptor 41 (GPR41). Proc Natl Acad Sci U S A 108(19):8030–8035. doi:10.1073/pnas.1016088108
Kimura I, Ozawa K, Inoue D, Imamura T, Kimura K, Maeda T, Terasawa K, Kashihara D, Hirano K, Tani T, Takahashi T, Miyauchi S, Shioi G, Inoue H, Tsujimoto G (2013) The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR43. Nat Commun 4:1829. doi:10.1038/ncomms2852
Koda S, Date Y, Murakami N, Shimbara T, Hanada T, Toshinai K, Niijima A, Furuya M, Inomata N, Osuye K, Nakazato M (2005) The role of the vagal nerve in peripheral PYY3-36-induced feeding reduction in rats. Endocrinology 146(5):2369–2375. doi:10.1210/en.2004-1266
Kotarsky K, Nilsson NE, Flodgren E, Owman C, Olde B (2003a) A human cell surface receptor activated by free fatty acids and thiazolidinedione drugs. Biochem Biophys Res Commun 301(2):406–410. doi:10.1016/s0006-291x(02)03064-4
Kotarsky K, Nilsson NE, Olde B, Owman C (2003b) Progress in methodology. Improved reporter gene assays used to identify ligands acting on orphan seven-transmembrane receptors. Pharmacol Toxicol 93(6):249–258
Lan H, Hoos LM, Liu L, Tetzloff G, Hu W, Abbondanzo SJ, Vassileva G, Gustafson EL, Hedrick JA, Davis HR (2008) Lack of FFAR1/GPR40 does not protect mice from high-fat diet-induced metabolic disease. Diabetes 57(11):2999–3006. doi:10.2337/db08-0596
Latour MG, Alquier T, Oseid E, Tremblay C, Jetton TL, Luo J, Lin DC, Poitout V (2007) GPR40 is necessary but not sufficient for fatty acid stimulation of insulin secretion in vivo. Diabetes 56(4):1087–1094. doi:10.2337/db06-1532
Le Poul E, Loison C, Struyf S, Springael JY, Lannoy V, Decobecq ME, Brezillon S, Dupriez V, Vassart G, Van Damme J, Parmentier M, Detheux M (2003) Functional characterization of human receptors for short chain fatty acids and their role in polymorphonuclear cell activation. J Biol Chem 278(28):25481–25489. doi:10.1074/jbc.M301403200
Leifke E, Naik H, Wu J, Viswanathan P, Demanno D, Kipnes M, Vakilynejad M (2012) A multiple-ascending-dose study to evaluate safety, pharmacokinetics, and pharmacodynamics of a novel GPR40 agonist, TAK-875, in subjects with type 2 diabetes. Clin Pharmacol Ther 92(1):29–39. doi:10.1038/clpt.2012.43
Ley RE, Turnbaugh PJ, Klein S, Gordon JI (2006) Microbial ecology: human gut microbes associated with obesity. Nature 444(7122):1022–1023. doi:10.1038/4441022a
Liaw CW, Connolly DT (2009) Sequence polymorphisms provide a common consensus sequence for GPR41 and GPR42. DNA Cell Biol 28(11):555–560. doi:10.1089/dna.2009.0916
Liou AP, Lu X, Sei Y, Zhao X, Pechhold S, Carrero RJ, Raybould HE, Wank S (2011) The G-protein-coupled receptor GPR40 directly mediates long-chain fatty acid-induced secretion of cholecystokinin. Gastroenterology 140(3):903–912. doi:10.1053/j.gastro.2010.10.012
Little TJ, Isaacs NJ, Young RL, Ott R, Nguyen NQ, Rayner CK, Horowitz M, Feinle-Bisset C (2014) Characterization of duodenal expression and localization of fatty acid-sensing receptors in humans: relationships with body mass index. Am J Physiol Gastrointest Liver Physiol 307(10):G958–G967. doi:10.1152/ajpgi.00134.2014
Luo J, Swaminath G, Brown SP, Zhang J, Guo Q, Chen M, Nguyen K, Tran T, Miao L, Dransfield PJ, Vimolratana M, Houze JB, Wong S, Toteva M, Shan B, Li F, Zhuang R, Lin DC (2012) A potent class of GPR40 full agonists engages the enteroinsular axis to promote glucose control in rodents. PLoS One 7(10):e46300. doi:10.1371/journal.pone.0046300
Ma D, Tao B, Warashina S, Kotani S, Lu L, Kaplamadzhiev DB, Mori Y, Tonchev AB, Yamashima T (2007) Expression of free fatty acid receptor GPR40 in the central nervous system of adult monkeys. Neurosci Res 58(4):394–401
Macia L, Tan J, Vieira AT, Leach K, Stanley D, Luong S, Maruya M, Ian McKenzie C, Hijikata A, Wong C, Binge L, Thorburn AN, Chevalier N, Ang C, Marino E, Robert R, Offermanns S, Teixeira MM, Moore RJ, Flavell RA, Fagarasan S, Mackay CR (2015) Metabolite-sensing receptors GPR43 and GPR109A facilitate dietary fibre-induced gut homeostasis through regulation of the inflammasome. Nat Commun 6:6734. doi:10.1038/ncomms7734
Mancini AD, Poitout V (2013) The fatty acid receptor FFA1/GPR40 a decade later: how much do we know? Trends Endocrinol Metab 24(8):398–407. doi:10.1016/j.tem.2013.03.003; S1043-2760(13)00050-7 [pii]
Martin C, Passilly-Degrace P, Chevrot M, Ancel D, Sparks SM, Drucker DJ, Besnard P (2012) Lipid-mediated release of GLP-1 by mouse taste buds from circumvallate papillae: putative involvement of GPR120 and impact on taste sensitivity. J Lipid Res 53(11):2256–2265. doi:10.1194/jlr.M025874
Marzuillo P, Grandone A, Conte M, Capuano F, Cirillo G, Di Sessa A, Umano GR, Romano R, Perrone L, del Giudice EM (2014) Novel association between a nonsynonymous variant (R270H) of the G-protein-coupled receptor 120 and liver injury in children and adolescents with obesity. J Pediatr Gastroenterol Nutr 59(4):472–475. doi:10.1097/MPG.0000000000000463
Maslowski KM, Vieira AT, Ng A, Kranich J, Sierro F, Yu D, Schilter HC, Rolph MS, Mackay F, Artis D, Xavier RJ, Teixeira MM, Mackay CR (2009) Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43. Nature 461(7268):1282–1286. doi:10.1038/nature08530
Masui R, Sasaki M, Funaki Y, Ogasawara N, Mizuno M, Iida A, Izawa S, Kondo Y, Ito Y, Tamura Y, Yanamoto K, Noda H, Tanabe A, Okaniwa N, Yamaguchi Y, Iwamoto T, Kasugai K (2013) G protein-coupled receptor 43 moderates gut inflammation through cytokine regulation from mononuclear cells. Inflamm Bowel Dis 19(13):2848–2856. doi:10.1097/01.MIB.0000435444.14860.ea
Matsumura S, Eguchi A, Mizushige T, Kitabayashi N, Tsuzuki S, Inoue K, Fushiki T (2009) Colocalization of GPR120 with phospholipase-Cbeta2 and alpha-gustducin in the taste bud cells in mice. Neurosci Lett 450(2):186–190. doi:10.1016/j.neulet.2008.11.056
McNelis JC, Lee YS, Mayoral R, van der Kant R, Johnson AM, Wollam J, Olefsky JM (2015) GPR43 potentiates beta-cell function in obesity. Diabetes 64(9):3203–3217. doi:10.2337/db14-1938
Mizuta K, Zhang Y, Mizuta F, Hoshijima H, Shiga T, Masaki E, Emala CW Sr (2015) Novel identification of the free fatty acid receptor FFAR1 that promotes contraction in airway smooth muscle. Am J Physiol Lung Cell Mol Physiol 309(9):L970–L982. doi:10.1152/ajplung.00041.2015
Moore K, Zhang Q, Murgolo N, Hosted T, Duffy R (2009) Cloning, expression, and pharmacological characterization of the GPR120 free fatty acid receptor from cynomolgus monkey: comparison with human GPR120 splice variants. Comp Biochem Physiol B Biochem Mol Biol 154(4):419–426. doi:10.1016/j.cbpb.2009.08.005
Nagasaki H, Kondo T, Fuchigami M, Hashimoto H, Sugimura Y, Ozaki N, Arima H, Ota A, Oiso Y, Hamada Y (2012) Inflammatory changes in adipose tissue enhance expression of GPR84, a medium-chain fatty acid receptor: TNFalpha enhances GPR84 expression in adipocytes. FEBS Lett 586(4):368–372. doi:10.1016/j.febslet.2012.01.001
Naik H, Vakilynejad M, Wu J, Viswanathan P, Dote N, Higuchi T, Leifke E (2012) Safety, tolerability, pharmacokinetics, and pharmacodynamic properties of the GPR40 agonist TAK-875: results from a double-blind, placebo-controlled single oral dose rising study in healthy volunteers. J Clin Pharmacol 52(7):1007–1016. doi:10.1177/0091270011409230; 0091270011409230 [pii]
Nilsson NE, Kotarsky K, Owman C, Olde B (2003) Identification of a free fatty acid receptor, FFA2R, expressed on leukocytes and activated by short-chain fatty acids. Biochem Biophys Res Commun 303(4):1047–1052. doi:10.1016/s0006-291x(03)00488-1
Nohr MK, Egerod KL, Christiansen SH, Gille A, Offermanns S, Schwartz TW, Moller M (2015) Expression of the short chain fatty acid receptor GPR41/FFAR3 in autonomic and somatic sensory ganglia. Neuroscience 290:126–137. doi:10.1016/j.neuroscience.2015.01.040
Offermanns S (2014) Free fatty acid (FFA) and hydroxy carboxylic acid (HCA) receptors. Annu Rev Pharmacol Toxicol 54:407–434. doi:10.1146/annurev-pharmtox-011613-135945
Ogawa T, Hirose H, Miyashita K, Saito I, Saruta T (2005) GPR40 gene Arg211His polymorphism may contribute to the variation of insulin secretory capacity in Japanese men. Metab Clin Exp 54(3):296–299. doi:10.1016/j.metabol.2004.09.008
Oh DY, Olefsky JM (2012) Omega 3 fatty acids and GPR120. Cell Metab 15(5):564–565. doi:10.1016/j.cmet.2012.04.009
Oh DY, Talukdar S, Bae EJ, Imamura T, Morinaga H, Fan W, Li P, Lu WJ, Watkins SM, Olefsky JM (2010) GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell 142(5):687–698. doi:10.1016/j.cell.2010.07.041
Pluznick J (2014) A novel SCFA receptor, the microbiota, and blood pressure regulation. Gut Microbes 5(2):202–207. doi:10.4161/gmic.27492
Pluznick JL, Protzko RJ, Gevorgyan H, Peterlin Z, Sipos A, Han J, Brunet I, Wan LX, Rey F, Wang T, Firestein SJ, Yanagisawa M, Gordon JI, Eichmann A, Peti-Peterdi J, Caplan MJ (2013) Olfactory receptor responding to gut microbiota-derived signals plays a role in renin secretion and blood pressure regulation. Proc Natl Acad Sci U S A 110(11):4410–4415. doi:10.1073/pnas.1215927110
Poitout V, Lin DC (2013) Modulating GPR40: therapeutic promise and potential in diabetes. Drug Discov Today 18(23–24):1301–1308. doi:10.1016/j.drudis.2013.09.003
Priyadarshini M, Layden BT (2015) FFAR3 modulates insulin secretion and global gene expression in mouse islets. Islets 7(2):e1045182. doi:10.1080/19382014.2015.1045182
Priyadarshini M, Villa SR, Fuller M, Wicksteed B, Mackay CR, Alquier T, Poitout V, Mancebo H, Mirmira RG, Gilchrist A, Layden BT (2015) An acetate-specific GPCR, FFAR2, regulates insulin secretion. Mol Endocrinol 29(7):1055–1066. doi:10.1210/me.2015-1007
Priyadarshini M, Wicksteed B, Schiltz GE, Gilchrist A, Layden BT (2016) SCFA receptors in pancreatic beta cells: novel diabetes targets? Trends Endocrinol Metab. doi:10.1016/j.tem.2016.03.011
Puhl HL 3rd, Won YJ, Lu VB, Ikeda SR (2015) Human GPR42 is a transcribed multisite variant that exhibits copy number polymorphism and is functional when heterologously expressed. Sci Rep 5:12880. doi:10.1038/srep12880
Regard JB, Sato IT, Coughlin SR (2008) Anatomical profiling of G protein-coupled receptor expression. Cell 135(3):561–571. doi:10.1016/j.cell.2008.08.040
Rodriguez-Pacheco F, Garcia-Serrano S, Garcia-Escobar E, Gutierrez-Repiso C, Garcia-Arnes J, Valdes S, Gonzalo M, Soriguer F, Moreno-Ruiz FJ, Rodriguez-Canete A, Gallego-Perales JL, Martinez-Ferriz A, Rojo-Martinez G, Garcia-Fuentes E (2014) Effects of obesity/fatty acids on the expression of GPR120. Mol Nutr Food Res 58(9):1852–1860. doi:10.1002/mnfr.201300666
Ryan KK, Seeley RJ (2013) Physiology. Food as a hormone. Science 339(6122):918–919. doi:10.1126/science.1234062
Salehi A, Flodgren E, Nilsson NE, Jimenez-Feltstrom J, Miyazaki J, Owman C, Olde B (2005) Free fatty acid receptor 1 (FFA(1)R/GPR40) and its involvement in fatty-acid-stimulated insulin secretion. Cell Tissue Res 322(2):207–215
Samuel BS, Shaito A, Motoike T, Rey FE, Backhed F, Manchester JK, Hammer RE, Williams SC, Crowley J, Yanagisawa M, Gordon JI (2008) Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein-coupled receptor, Gpr41. Proc Natl Acad Sci U S A 105(43):16767–16772. doi:10.1073/pnas.0808567105
Sawzdargo M, George SR, Nguyen T, Xu S, Kolakowski LF, O’Dowd BF (1997) A cluster of four novel human G protein-coupled receptor genes occurring in close proximity to CD22 gene on chromosome 19q13.1. Biochem Biophys Res Commun 239(2):543–547
Schnell S, Schaefer M, Schofl C (2007) Free fatty acids increase cytosolic free calcium and stimulate insulin secretion from beta-cells through activation of GPR40. Mol Cell Endocrinol 263(1–2):173–180. doi:10.1016/j.mce.2006.09.013
Sekiguchi H, Kasubuchi M, Hasegawa S, Pelisch N, Kimura I, Ichimura A (2015) A novel antidiabetic therapy: free fatty acid receptors as potential drug target. Curr Diabetes Rev 11(2):107–115
Sina C, Gavrilova O, Forster M, Till A, Derer S, Hildebrand F, Raabe B, Chalaris A, Scheller J, Rehmann A, Franke A, Ott S, Hasler R, Nikolaus S, Folsch UR, Rose-John S, Jiang HP, Li J, Schreiber S, Rosenstiel P (2009) G protein-coupled receptor 43 is essential for neutrophil recruitment during intestinal inflammation. J Immunol 183(11):7514–7522. doi:10.4049/jimmunol.0900063
Smith NJ, Stoddart LA, Devine NM, Jenkins L, Milligan G (2009) The action and mode of binding of thiazolidinedione ligands at free fatty acid receptor 1. J Biol Chem 284(26):17527–17539. doi:10.1074/jbc.M109.012849
Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly YM, Glickman JN, Garrett WS (2013) The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 341(6145):569–573. doi:10.1126/science.1241165
Spector AA, Kim HY (2014) Discovery of essential fatty acids. J Lipid Res. doi:10.1194/jlr.R055095
Steneberg P, Rubins N, Bartoov-Shifman R, Walker MD, Edlund H (2005) The FFA receptor GPR40 links hyperinsulinemia, hepatic steatosis, and impaired glucose homeostasis in mouse. Cell Metab 1(4):245–258. doi:10.1016/j.cmet.2005.03.007
Stoddart LA, Smith NJ, Jenkins L, Brown AJ, Milligan G (2008a) Conserved polar residues in transmembrane domains V, VI, and VII of free fatty acid receptor 2 and free fatty acid receptor 3 are required for the binding and function of short chain fatty acids. J Biol Chem 283(47):32913–32924. doi:10.1074/jbc.M805601200
Stoddart LA, Smith NJ, Milligan G (2008b) International Union of Pharmacology. LXXI. Free fatty acid receptors FFA1, -2, and -3: pharmacology and pathophysiological functions. Pharmacol Rev 60(4):405–417. doi:10.1124/pr.108.00802
Stone VM, Dhayal S, Brocklehurst KJ, Lenaghan C, Sorhede Winzell M, Hammar M, Xu X, Smith DM, Morgan NG (2014) GPR120 (FFAR4) is preferentially expressed in pancreatic delta cells and regulates somatostatin secretion from murine islets of Langerhans. Diabetologia 57(6):1182–1191. doi:10.1007/s00125-014-3213-0
Stumvoll M, Haring H (2002) The peroxisome proliferator-activated receptor-gamma2 Pro12Ala polymorphism. Diabetes 51(8):2341–2347
Suckow AT, Polidori D, Yan W, Chon S, Ma JY, Leonard J, Briscoe CP (2014) Alteration of the glucagon axis in GPR120 (FFAR4) knockout mice: a role for GPR120 in glucagon secretion. J Biol Chem 289(22):15751–15763. doi:10.1074/jbc.M114.568683
Sum CS, Tikhonova IG, Neumann S, Engel S, Raaka BM, Costanzi S, Gershengorn MC (2007) Identification of residues important for agonist recognition and activation in GPR40. J Biol Chem 282(40):29248–29255. doi:10.1074/jbc.M705077200
Suzuki M, Takaishi S, Nagasaki M, Onozawa Y, Iino I, Maeda H, Komai T, Oda T (2013) Medium-chain fatty acid-sensing receptor, GPR84, is a proinflammatory receptor. J Biol Chem 288(15):10684–10691. doi:10.1074/jbc.M112.420042
Sykaras AG, Demenis C, Case RM, McLaughlin JT, Smith CP (2012) Duodenal enteroendocrine I-cells contain mRNA transcripts encoding key endocannabinoid and fatty acid receptors. PLoS One 7(8):e42373. doi:10.1371/journal.pone.0042373
Takano R, Yoshida M, Inoue M, Honda T, Nakashima R, Matsumoto K, Yano T, Ogata T, Watanabe N, Toda N (2014) Discovery of 3-aryl-3-ethoxypropanoic acids as orally active GPR40 agonists. Bioorg Med Chem Lett 24(13):2949–2953. doi:10.1016/j.bmcl.2014.04.065
Taneera J, Lang S, Sharma A, Fadista J, Zhou Y, Ahlqvist E, Jonsson A, Lyssenko V, Vikman P, Hansson O, Parikh H, Korsgren O, Soni A, Krus U, Zhang E, Jing XJ, Esguerra JL, Wollheim CB, Salehi A, Rosengren A, Renstrom E, Groop L (2012) A systems genetics approach identifies genes and pathways for type 2 diabetes in human islets. Cell Metab 16(1):122–134. doi:10.1016/j.cmet.2012.06.006
Tang Y, Chen Y, Jiang H, Robbins GT, Nie D (2011) G-protein-coupled receptor for short-chain fatty acids suppresses colon cancer. Int J Cancer 128(4):847–856. doi:10.1002/ijc.25638
Tang C, Ahmed K, Gille A, Lu S, Grone HJ, Tunaru S, Offermanns S (2015) Loss of FFA2 and FFA3 increases insulin secretion and improves glucose tolerance in type 2 diabetes. Nat Med 21(2):173–177. doi:10.1038/nm.3779
Tazoe H, Otomo Y, Kaji I, Tanaka R, Karaki SI, Kuwahara A (2008) Roles of short-chain fatty acids receptors, GPR41 and GPR43 on colonic functions. J Physiol Pharmacol 59(Suppl 2):251–262
Tazoe H, Otomo Y, Karaki S, Kato I, Fukami Y, Terasaki M, Kuwahara A (2009) Expression of short-chain fatty acid receptor GPR41 in the human colon. Biomed Res 30(3):149–156
Tolhurst G, Heffron H, Lam YS, Parker HE, Habib AM, Diakogiannaki E, Cameron J, Grosse J, Reimann F, Gribble FM (2012) Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes 61(2):364–371. doi:10.2337/db11-1019
Trompette A, Gollwitzer ES, Yadava K, Sichelstiel AK, Sprenger N, Ngom-Bru C, Blanchard C, Junt T, Nicod LP, Harris NL, Marsland BJ (2014) Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat Med 20(2):159–166. doi:10.1038/nm.3444
Tsujihata Y, Ito R, Suzuki M, Harada A, Negoro N, Yasuma T, Momose Y, Takeuchi K (2011) TAK-875, an orally available G protein-coupled receptor 40/free fatty acid receptor 1 agonist, enhances glucose-dependent insulin secretion and improves both postprandial and fasting hyperglycemia in type 2 diabetic rats. J Pharmacol Exp Ther 339(1):228–237. doi:10.1124/jpet.111.183772; jpet.111.183772 [pii]
Turton MD, O’Shea D, Gunn I, Beak SA, Edwards CM, Meeran K, Choi SJ, Taylor GM, Heath MM, Lambert PD, Wilding JP, Smith DM, Ghatei MA, Herbert J, Bloom SR (1996) A role for glucagon-like peptide-1 in the central regulation of feeding. Nature 379(6560):69–72. doi:10.1038/379069a0
Ulven T, Christiansen E (2015) Dietary fatty acids and their potential for controlling metabolic diseases through activation of FFA4/GPR120. Annu Rev Nutr 35:239–263. doi:10.1146/annurev-nutr-071714-034410
Vestmar MA, Andersson EA, Christensen CR, Hauge M, Glumer C, Linneberg A, Witte DR, Jorgensen ME, Christensen C, Brandslund I, Lauritzen T, Pedersen O, Holst B, Grarup N, Schwartz TW, Hansen T (2016) Functional and genetic epidemiological characterisation of the FFAR4 (GPR120) p.R270H variant in the Danish population. J Med Genet. doi:10.1136/jmedgenet-2015-103728
Vettor R, Granzotto M, De Stefani D, Trevellin E, Rossato M, Farina MG, Milan G, Pilon C, Nigro A, Federspil G, Vigneri R, Vitiello L, Rizzuto R, Baratta R, Frittitta L (2008) Loss-of-function mutation of the GPR40 gene associates with abnormal stimulated insulin secretion by acting on intracellular calcium mobilization. J Clin Endocrinol Metab 93(9):3541–3550. doi:10.1210/jc.2007-2680
Vinolo MA, Ferguson GJ, Kulkarni S, Damoulakis G, Anderson K, Bohlooly YM, Stephens L, Hawkins PT, Curi R (2011) SCFAs induce mouse neutrophil chemotaxis through the GPR43 receptor. PLoS One 6(6):e21205. doi:10.1371/journal.pone.0021205
Wagner R, Kaiser G, Gerst F, Christiansen E, Due-Hansen ME, Grundmann M, Machicao F, Peter A, Kostenis E, Ulven T, Fritsche A, Haring HU, Ullrich S (2013) Reevaluation of fatty acid receptor 1 as a drug target for the stimulation of insulin secretion in humans. Diabetes 62(6):2106–2111. doi:10.2337/db12-1249
Wagner R, Hieronimus A, Lamprinou A, Heni M, Hatziagelaki E, Ullrich S, Stefan N, Staiger H, Haring HU, Fritsche A (2014) Peroxisome proliferator-activated receptor gamma (PPARG) modulates free fatty acid receptor 1 (FFAR1) dependent insulin secretion in humans. Mol Metab 3(6):676–680. doi:10.1016/j.molmet.2014.07.001
Waguri T, Goda T, Kasezawa N, Yamakawa-Kobayashi K (2013) The combined effects of genetic variations in the GPR120 gene and dietary fat intake on obesity risk. Biomed Res 34(2):69–74
Watson SJ, Brown AJ, Holliday ND (2012) Differential signaling by splice variants of the human free fatty acid receptor GPR120. Mol Pharmacol 81(5):631–642. doi:10.1124/mol.111.077388
Watterson KR, Hudson BD, Ulven T, Milligan G (2014) Treatment of type 2 diabetes by free fatty acid receptor agonists. Front Endocrinol 5:137. doi:10.3389/fendo.2014.00137
Xiong Y, Miyamoto N, Shibata K, Valasek MA, Motoike T, Kedzierski RM, Yanagisawa M (2004) Short-chain fatty acids stimulate leptin production in adipocytes through the G protein-coupled receptor GPR41. Proc Natl Acad Sci U S A 101(4):1045–1050. doi:10.1073/pnas.2637002100
Yabuki C, Komatsu H, Tsujihata Y, Maeda R, Ito R, Matsuda-Nagasumi K, Sakuma K, Miyawaki K, Kikuchi N, Takeuchi K, Habata Y, Mori M (2013) A novel antidiabetic drug, fasiglifam/TAK-875, acts as an ago-allosteric modulator of FFAR1. PLoS One 8(10):e76280. doi:10.1371/journal.pone.0076280
Yonezawa T, Kobayashi Y, Obara Y (2007) Short-chain fatty acids induce acute phosphorylation of the p38 mitogen-activated protein kinase/heat shock protein 27 pathway via GPR43 in the MCF-7 human breast cancer cell line. Cell Signal 19(1):185–193. doi:10.1016/j.cellsig.2006.06.004
Zaibi MS, Stocker CJ, O’Dowd J, Davies A, Bellahcene M, Cawthorne MA, Brown AJ, Smith DM, Arch JR (2010) Roles of GPR41 and GPR43 in leptin secretory responses of murine adipocytes to short chain fatty acids. FEBS Lett 584(11):2381–2386. doi:10.1016/j.febslet.2010.04.027
Zhou SF, Liu JP, Chowbay B (2009) Polymorphism of human cytochrome P450 enzymes and its clinical impact. Drug Metab Rev 41(2):89–295. doi:10.1080/03602530902843483
Conflict of Interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Ichimura, A. (2016). Polymorphic Variation in FFA Receptors: Functions and Consequences. In: Milligan, G., Kimura, I. (eds) Free Fatty Acid Receptors. Handbook of Experimental Pharmacology, vol 236. Springer, Cham. https://doi.org/10.1007/164_2016_57
Download citation
DOI: https://doi.org/10.1007/164_2016_57
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-50692-0
Online ISBN: 978-3-319-50693-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)