Abstract
There is an urgent unmet medical need for new antibiotics for wound and burn infections caused by multidrug-resistant (MDR) Gram-negative ‘superbugs’ Pseudomonas aeruginosa, Acinetobacter baumannii and Klebsiella pneumoniae. The authors discuss the development of novel broad-spectrum lipopeptides that are very active against not only polymyxin-resistant Gram-negative pathogens but also MDR Gram-positive Staphylococcus aureus and Enterococcus faecium that also commonly cause serious wound infections. The authors describe MDR bacterial wound infections, mechanisms of polymyxin activity and resistance and the discovery of new polymyxin-like lipopeptides targeting MDR ‘superbugs’. These next-generation polymyxins hold significant potential for the treatment of chronic wound infections caused by problematic Gram-negative ‘superbugs’.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
The annual costs of wound care in Australia ($2.6 billion AUD), the UK (£2.3–3.1 billion) and the USA ($50 billion USD) are staggering. The cost of chronic wound infections is often due to lengthy hospitalisations because of infections caused by multidrug-resistant (MDR) bacterial pathogens [1]. There is an urgent unmet medical need for new antibiotics for wound and burn infections caused by MDR Gram-negative ‘superbugs’ Pseudomonas aeruginosa, Acinetobacter baumannii and Klebsiella pneumoniae. Resistance to the last-line therapy polymyxins (polymyxin B and colistin) has been increasingly reported, which virtually means no antibiotic will be available for treatment of wound and burn infections. Considering potential systemic toxicity and suboptimal pharmacokinetic/pharmacodynamic attainment, the topical use of antibiotics often remains a superior approach for wound infections than parenteral administration.
The present chapter covers the development of novel broad-spectrum lipopeptides that are very active against not only polymyxin-resistant Gram-negative pathogens but also MDR Gram-positive Staphylococcus aureus and Enterococcus faecium that also commonly cause serious wound infections. Furthermore, we have developed a chitosan-based colistin self-healable hydrogel that provides high localised release of colistin for the treatment of burn wound infections. The development of these novel topical lipopeptide agents could slash the billion-dollar annual cost of wound treatment and result in improved healthcare on a global scale.
2 MDR Bacterial Wound Infections
Wound and burn infections are a major medical challenge worldwide and represent a considerable healthcare burden [2,3,4]. They are a common risk for patients with chronic non-healing wounds which cause high morbidity and mortality. As a poignant example, ~75% of all deaths following major burn injuries are related to bacterial infections [3, 4]. Wound and burn infections caused by the aforementioned Gram-negative ‘superbugs’ are immensely concerning [5]. Burns are particularly susceptible to infections due to the disruption of the epidermal barrier, the systemic apoptotic response and immunosuppression that disrupts self-defence mechanisms to fight infection [3, 6]. Even though systemic antibiotic treatment is usually the most common therapeutic option, the significant difficulties are adverse effects and the risk of an insufficient tissue penetration due to impaired blood circulation. The use of topical chemotherapy has been fundamental and helped to improve the survival of patients with major burns and to minimise the incidence of life-threatening burn wound sepsis [7]. The topical use of antibiotics plays a significant role in the management of serious wound infections caused by Gram-negative bacteria P. aeruginosa, A. baumannii and K. pneumoniae and Gram-positive S. aureus and E. faecium [3, 4]. Very worryingly, these bacteria are increasingly resistant to almost all current topical antibiotics [8, 9]. These bacterial ‘superbugs’ have been identified by the Infectious Diseases Society of America (IDSA) and Centre for Disease Control and Prevention (CDC) as the top-priority dangerous ‘superbugs’ that require urgent attention for discovery of novel antibiotics [10,11,12,13].
Polymyxins are an important last-line therapy against Gram-negative ‘superbugs’.
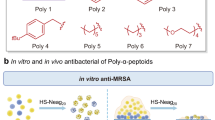
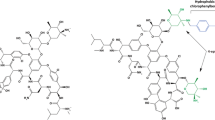
Polymyxins consist of a linear tripeptide fragment having an N-terminal fatty acyl tail attached to a cyclic heptapeptide (Fig. 24.1). They are polycations at pH 7.4 owing to the five diaminobutyric acid (Dab) residues. Polymyxins were discovered more than 60 years ago. Because the early experience in the 1960s with parenteral polymyxins led to some cases of nephrotoxicity and neurotoxicity, their clinical use waned [14,15,16,17]. Since the mid-1990s, there has been a greatly renewed interest in polymyxins because of the increasing prevalence of MDR P. aeruginosa, A. baumannii and K. pneumoniae [14,15,16,17]. Polymyxin B and colistin (polymyxin E) are the two clinically available polymyxins that are most commonly administered parenterally in patients as a last-line therapy for serious infections, when all other available antibiotics are inactive. Our in vitro studies have shown that resistance can rapidly emerge in P. aeruginosa, A. baumannii and K. pneumoniae [18,19,20], and polymyxin resistance in hospitalised patients has been increasingly reported [10, 21, 22]. Even more worrying is the recent reports in the Lancet Infect Dis of the emergence of plasmid-mediated colistin resistance [23, 24], which implies resistance to these important last-line antibiotics can now rapidly spread. Resistance to polymyxins implies a total lack of antibiotics for treatment of life-threatening Gram-negative infections.
The majority of the modern pharmacological data of polymyxins are obtained by our group [18, 20, 25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]. We were the first to characterise the modern pharmacokinetics of colistin and polymyxin B in patients [25, 30, 39, 40] and demonstrate that polymyxins exhibit rapid, concentration-dependent killing of susceptible strains of P. aeruginosa, A. baumannii and K. pneumoniae [20, 34, 41]. Our studies in both in vitro and animal infection models have, for the first time, elucidated that fAUC/MIC (i.e. ratio of the area under the free plasma concentration—time curve to minimal inhibitory concentration [MIC]) is the pharmacokinetic/pharmacodynamic (PK/PD) index best correlating with colistin activity [44]. Our findings are led to the first scientifically based dosage regimens in patients. Our recent data suggest that intravenous polymyxins are not ideal for treatment of lung infections and wound infections due to suboptimal PK/PD exposure at infection sites. We first reported colistin heteroresistance (i.e. colistin-resistant subpopulations in an isolate susceptible based upon MIC) in the Gram-negative pathogens [20, 31, 36] and the potential for resistant subpopulations to rapidly amplify upon exposure to colistin in an in vitro PK/PD model that mimics clinical dosing regimens in humans [18,19,20]. The latter highlights the urgency to develop new antibiotics active against isolates which are resistant to polymyxins and all other current antibiotics.
3 Mechanisms of Polymyxin Activity and Resistance
The initial cellular target of polymyxins is the lipid A component of lipopolysaccharide (LPS) in the outer membrane (OM). The purported primary mechanism of polymyxin activity involves an initial electrostatic interaction of the cationic Dab residues of the polymyxin molecule with the negatively charged phosphate groups of lipid A [45]. This initial polar interaction is followed by insertion of the fatty acyl tail of the polymyxin into the lipid A fatty acyl layer in the outer membrane. Many of the Gram-negative bacterial mechanisms of resistance to polymyxins are based on modifications to lipid A which reduce or abolish this initial electrostatic interaction. Modification of the phosphates of lipid A with positively charged moieties such as 4-amino-4-deoxy-L-arabinose or phosphoethanolamine reduces the net negative charge of lipid A, thereby increasing resistance to polymyxins [46,47,48,49,50,51,52,53].
4 Discovery of New Polymyxin-Like Lipopeptides Targeting MDR ‘Superbugs’
We were invited by the Journal of Medicinal Chemistry to review the current state of development of polymyxin analogues [54]. Previous medicinal chemistry strategies for improving the antibacterial activity of polymyxins have been empirical and limited to modifications of the Dab residues, the heptapeptide ring and the length of the N-terminal fatty acyl chain (Fig. 1) [55,56,57,58,59,60]. Notably, numerous attempts have been made to modify the N-terminus with polar and lipophilic groups but with little success [54]. One such notable N-terminal analogue (CB-182804) came from Cubist; unfortunately this analogue failed in a Phase 1 clinical trial. Importantly, CB-182804 was not active against any polymyxin-resistant isolates [61]. None of the previous discovery programmes were specifically driven by an SAR approach nor was polymyxin resistance targeted. These major shortcomings led to the failure of the novel polymyxin discovery programmes by Cubist, AstraZeneca and Pfizer. To the best of our knowledge, we are the first to apply an SAR-based mechanistic model (Fig. 2) to discover novel lipopeptides against polymyxin-resistant Gram-negative ‘superbugs’ [62]. The SAR model has allowed us to identify key structural properties of polymyxins that confer antibacterial activity. In our model, the polymyxin-lipid A complex is stabilised by a combination of polar and hydrophobic interactions (Fig. 2). The positive charges on Dab1 and Dab5 of polymyxin B interact with the negatively charged 4′-phosphate group of lipid A, and Dab8 and Dab9 similarly interact with the 1-phosphate of lipid A. The polymyxin-lipid A complex is further stabilised by hydrophobic contacts between the N-terminal fatty acyl chain and position 6/7 D-Phe-L-Leu segment of the polymyxin molecule, with the fatty acyl chains of lipid A. Evidently, the SAR model indicates that the polymyxin-lipid A interaction in both polymyxin-susceptible and polymyxin-resistant strains can be significantly accentuated through the introduction of additional hydrophobic contacts. To circumvent bacterial resistance mechanisms due to modifications of lipid A, in one series of our novel FADDI lipopeptides, hydrophobic modifications were introduced at position 6 or 7 to enhance penetration into the lipid A fatty acyl layer as suggested by the SAR model (Fig. 2). The SAR model was validated when our first generation lipopeptides (e.g. FADDI-002) (Table 1) with L-octylglycine substituted at position 7 displayed potent antimicrobial activity against polymyxin-resistant Gram-negative clinical isolates [62]. Subsequently, expansion of our SAR-based design strategy to include compounds incorporating lipidic groups at position 6 and the N-terminus also generated potent lipopeptides active against polymyxin-resistant Gram-negative ‘superbugs’ (Table 1). Notably, FADDI-019 and FADDI-020 which have the same or very similar MICs (1–4 mg/L) as colistin against colistin-susceptible P. aeruginosa isolates displayed significant activity (MICs 1–4 mg/L) against colistin-resistant P. aeruginosa (colistin MICs 32 or >128 mg/L). In static time-killing studies, FADDI-019 (MIC 1 mg/L) at 4 × MIC achieved ~6 log10 kill against a polymyxin-resistant MDR clinical P. aeruginosa isolate (colistin MIC >128 mg/L) with no viable cells detected even at 2 h; no killing was observed with colistin even at 32 mg/L. Against polymyxin-susceptible P. aeruginosa ATCC 27853 (colistin MIC 1 mg/L), FADDI-019 (MIC 1 mg/L) had comparable bacterial time-kill to colistin. For most of our lipopeptides, the ratios of MBCs (minimal bactericidal concentrations) to MICs were ≤4 indicating a low potential for development of resistance. Isothermal titration calorimetry studies confirmed that the hydrophobic contribution from the N-terminal fatty acyl chain is the predominant driving force for polymyxin-lipid A complexation [63, 64].
Serendipitously, a series of our lipopeptides have unexpected activity against MDR Gram-positive S. aureus and E. faecium which are intrinsically resistant to polymyxins (colistin and polymyxin B MIC >128 mg/L). Transcriptome analysis using RNA-seq revealed that virulence determinants controlled by SaeRS and the expression of enterotoxins yent2, sei, sem and seo were all significantly downregulated by FADDI-019 [65]. Clearly, our SAR-based mechanistic model has led to unique opportunities to optimise the polymyxin structure to overcome both adaptive and intrinsic resistance to current polymyxins. There was no haemolysis in human red blood cells treated with the tested FADDI lipopeptides or polymyxins at 128 mg/L (the highest concentration examined). After administration of FADDI-002, FADDI-003, FADDI-019 or FADDI-020 to rats (intravenous, 0.75 mg/kg) and mice (subcutaneous, 40 mg/kg), no adverse effects were observed.
Preliminary in vitro studies to examine the impact of the lipopeptides on human keratinocytes and murine fibroblast cells, polymyxin B, FADDI-019 and FADDI-073 at 1.5, 5, 15 and 50 mg/L had little effect over 48 h on the morphology of fibroblasts (3 T3) and keratinocytes (HaCaT). FADDI-019, FADDI-073 and polymyxin B stimulated metabolic activity above mock-treated cultures in 3T3 cells in a dose-dependent manner at 24 and 48 h. However, similar responses were not observed in HaCaT cells; neither FADDI-019 nor FADDI-073 affected the cellular metabolic activity at any of the four concentrations at 24 or 48 h, while only 1.5 and 5 mg/L polymyxin B slightly decreased the cellular metabolic activity at both time points. It is noteworthy that for many years a topical formulation containing polymyxin B has been used for treating skin infections, with negligible toxicity [66]. Our results suggest that our lipopeptides have at least similar tolerability to colistin and polymyxin B.
5 Synthesis of a Chitosan-Colistin Hydrogel and Testing in a Mouse Burn Infection Model
We have synthesised a chitosan-colistin hydrogel and assessed its efficacy in a mouse burn infection model (Fig. 3) [67]. The chitosan-colistin hydrogel is an inexpensive, self-healable and highly biocompatible material which provides up to 95% colistin release within 24 h and showed excellent in vitro activity against P. aeruginosa in a disc diffusion assay. The physical properties of the hydrogel were unaffected by colistin; this allowed us to load a wide range of colistin concentrations into the hydrogel matrix without impacting its size. Serendipitously, the hydrogel formation process was accelerated in the presence of colistin. Excitingly, the chitosan-colistin hydrogel dressing (containing 0.3 mg colistin) displayed excellent in vivo activity, producing a ~4 log reduction in the bacterial load in a burn wound (1 cm2) infection, established in mice by inoculating 100 μL 108 CFU/mL of P. aeruginosa ATCC 27853. We are currently exploring lipopeptide-hydrogel dressing systems using the superior FADDI lipopeptides, for which formulation characteristics (e.g. lipopeptide loading and mechanical properties) will be investigated and optimised.
Silk proteins serve as excellent scaffolds for wound healing and in tissue engineering [68].
Steinstraesser et al. [68] loaded ST-silk protein membranes (thickness, 100 μm; pore size, <100 nm) with colistin (0.027–270 mg/mL) and examined their efficacy against P. aeruginosa in animal wound infection models. The ST-silk membranes loaded with 270 mg/mL colistin demonstrated a > 3 log reduction in colony-forming units of P. aeruginosa ATCC 27853 after 4 days (~25-fold decrease from the carrier control). Similarly, in a porcine wound infection model, the ST-silk membranes loaded with 270 mg/mL colistin demonstrated an almost complete clearance of the infection after the entire follow-up of 6 days.
6 Perspective
The World Health Organization has identified antimicrobial resistance as one of the three greatest threats to human health. The last-line therapy polymyxins are losing their activity; however, no new antibiotic will be available for many years to come. The prevalence of wound infections caused by the bacterial ‘superbugs’ highlights the urgency of discovering novel antibiotics for topical treatment of serious wound infections. As the Infectious Diseases Society of America highlighted, ‘as antibiotic discovery stagnates, a public health crisis brews’, the recent emergence of plasmid-borne resistance to the last-line polymyxins highlights the urgency to develop novel antibiotics to combat these very problematic pathogens. This chapter details the development of novel polymyxin lipopeptides and hydrogel formulations as new antibiotics for topical use in wound treatment against problematic ‘superbugs’ that are resistant to all current antibiotics. These next-generation polymyxins hold significant potential for the treatment of chronic wound infections caused by problematic Gram-negative ‘superbugs’.
References
Whitlock E, Morcom J, Spurling G, Janamian T, Ryan S (2014) Wound care costs in general practice—a cross-sectional study. Aust Fam Physician 43:143–146
Jacobsen F, Fisahn C, Sorkin M, Thiele I, Hirsch T, Stricker I, Klaassen T, Roemer A, Fugmann B, Steinstraesser L (2011) Efficacy of topically delivered moxifloxacin against wound infection by Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 55:2325–2334
Church D, Elsayed S, Reid O, Winston B, Lindsay R (2006) Burn wound infections. Clin Microbiol Rev 19:403–434
Vindenes H, Bjerknes R (1995) Microbial colonization of large wounds. Burns 21:575–579
Bad bugs, no drugs. https://www.idsociety.org/uploadedFiles/IDSA/Policy_and_Advocacy/Current_Topics_and_Issues/Advancing_Product_Research_and_Development/Bad_Bugs_No_Drugs/Statements/As%20Antibiotic%20Discovery%20Stagnates%20A%20Public%20Health%20Crisis%20Brews.pdf. Accessed 21 Mar 2017
Gravante G, Delogu D, Sconocchia G (2007) “Systemic apoptotic response” after thermal burns. Apoptosis 12:259–270
Honari S (2004) Topical therapies and antimicrobials in the management of burn wounds. Crit Care Nurs Clin North Am 16:1–11
Thomas CM, Hothersall J, Willis CL, Simpson TJ (2010) Resistance to and synthesis of the antibiotic mupirocin. Nat Rev Microbiol 8:281–289
Sevgi M, Toklu A, Vecchio D et al (2013) Topical antimicrobials for burn infections – an update. Recent Pat Antiinfect Drug Discov 8:161–197
Talbot GH, Bradley J, Edwards JE Jr, Gilbert D, Scheld M, Bartlett JG, Antimicrobial availability task force of the infectious diseases society of America (2006) Bad bugs need drugs: an update on the development pipeline from the Antimicrobial Availability Task Force of the Infectious Diseases Society of America. Clin Infect Dis 42:657–668
Boucher HW, Talbot GH, Bradley JS, Edwards JE, Gilbert D, Rice LB, Scheld M, Spellberg B, Bartlett J (2009) Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis 48:1–12
Gilbert DN, Guidos RJ, Boucher HW, Talbot GH, Spellberg B, Edwards JE Jr, Scheld WM, Bradley JS, Bartlett JG (2010) The 10 × 20 Initiative: Pursuing a global commitment to develop 10 new antibacterial drugs by 2020. Clin Infect Dis 50:1081–1083
Centers for Disease Control and Prevention (2013) Antibiotic resistance threats in the United States
Evans ME, Feola DJ, Rapp RP (1999) Polymyxin B sulfate and colistin: old antibiotics for emerging multiresistant gram-negative bacteria. Ann Pharmacother 33:960–967
Falagas ME, Kasiakou SK (2005) Colistin: the revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clin Infect Dis 40:1333–1341
Landman D, Georgescu C, Martin DA et al (2008) Polymyxins revisited. Clin Microbiol Rev 21:449–465
Zavascki AP, Goldani LZ, Li J, Nation RL (2007) Polymyxin B for the treatment of multidrug-resistant pathogens: a critical review. J Antimicrob Chemother 60:1206–1215
Bergen PJ, Tsuji BT, Bulitta JB, Forrest A, Jacob J, Sidjabat HE, Paterson DL, Nation RL, Li J (2011) Synergistic killing of multidrug-resistant Pseudomonas aeruginosa at multiple inocula by colistin combined with doripenem in an in vitro pharmacokinetic/pharmacodynamic model. Antimicrob Agents Chemother 55:5685–5695
Tan CH, Li J, Nation RL (2007) Activity of colistin against heteroresistant Acinetobacter baumannii and emergence of resistance in an in vitro pharmacokinetic/pharmacodynamic model. Antimicrob Agents Chemother 51:3413–3415
Poudyal A, Howden BP, Bell JM, Gao W, Owen RJ, Turnidge JD, Nation RL, Li J (2008) In vitro pharmacodynamics of colistin against multidrug-resistant Klebsiella pneumoniae. J Antimicrob Chemother 62:1311–1318
Gales AC, Jones RN, Sader HS (2011) Contemporary activity of colistin and polymyxin B against a worldwide collection of Gram-negative pathogens: results from the SENTRY Antimicrobial Surveillance Program (2006–09). J Antimicrob Chemother 66:2070–2074
Paterson DL, Lipman J (2007) Returning to the pre-antibiotic era in the critically ill: the XDR problem. Crit Care Med 35:1789–1791
Liu YY, Wang Y, Walsh TR, Yi LX, Zhang R, Spencer J, Doi Y, Tian G, Dong B, Huang X, Yu LF, Gu D, Ren H, Chen X, Lv L, He D, Zhou H, Liang Z, Liu JH, Shen J (2016) Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis 16(2):161–168
Webb HE, Granier SA, Marault M, Millemann Y, den Bakker HC, Nightingale KK, Bugarel M, Ison SA, Scott HM, Loneragan GH (2016) Dissemination of the mcr-1 colistin resistance gene. Lancet Infect Dis 16:144–145
Li J, Coulthard K, Milne R, Nation RL, Conway S, Peckham D, Etherington C, Turnidge J (2003) Steady-state pharmacokinetics of intravenous colistin methanesulfonate in patients with cystic fibrosis. J Antimicrob Chemother 52:987–992
Li J, Milne RW, Nation RL, Turnidge JD, Smeaton TC, Coulthard K (2003) Use of high-performance liquid chromatography to study the pharmacokinetics of colistin sulfate in rats following intravenous administration. Antimicrob Agents Chemother 47:1766–1770
Li J, Milne RW, Nation RL, Turnidge JD, Smeaton TC, Coulthard K (2004) Pharmacokinetics of colistin methanesulphonate and colistin in rats following an intravenous dose of colistin methanesulphonate. J Antimicrob Chemother 53:837–840
Li J, Nation RL, Owen RJ, Wong S, Spelman D, Franklin C (2007) Antibiograms of multidrug-resistant clinical Acinetobacter baumannii: promising therapeutic options for treatment of infection with colistin-resistant strains. Clin Infect Dis 45:594–598
Li J, Nation RL, Turnidge JD, Milne RW, Coulthard K, Rayner CR, Paterson DL (2006) Colistin: the re-emerging antibiotic for multidrug-resistant Gram-negative bacterial infections. Lancet Infect Dis 6:589–601
Li J, Rayner CR, Nation RL, Deans R, Boots R, Widdecombe N, Douglas A, Lipman J (2005) Pharmacokinetics of colistin methanesulfonate and colistin in a critically ill patient receiving continuous venovenous hemodiafiltration. Antimicrob Agents Chemother 49:4814–4815
Li J, Rayner CR, Nation RL, Owen RJ, Spelman D, Tan KE, Liolios L (2006) Heteroresistance to colistin in multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother 50:2946–2950
Dudhani RV, Turnidge JD, Coulthard K, Milne RW, Rayner CR, Li J, Nation RL (2010) Elucidation of the pharmacokinetic/pharmacodynamic determinant of colistin activity against Pseudomonas aeruginosa in murine thigh and lung infection models. Antimicrob Agents Chemother 54:1117–1124
Dudhani RV, Turnidge JD, Nation RL, Li J (2010) fAUC/MIC is the most predictive pharmacokinetic/pharmacodynamic index of colistin against Acinetobacter baumannii in murine thigh and lung infection models. J Antimicrob Chemother 65:1984–1990
Owen RJ, Li J, Nation RL, Spelman D (2007) In vitro pharmacodynamics of colistin against Acinetobacter baumannii clinical isolates. J Antimicrob Chemother 59:473–477
Bergen PJ, Bulitta JB, Forrest A, Tsuji BT, Li J, Nation RL (2010) Pharmacokinetic/pharmacodynamic investigation of colistin against Pseudomonas aeruginosa using an in vitro model. Antimicrob Agents Chemother 54(9):3783
Bergen PJ, Forrest A, Bulitta JB, Tsuji BT, Sidjabat HE, Paterson DL, Li J, Nation RL (2011) Clinically relevant plasma concentrations of colistin in combination with imipenem enhance pharmacodynamic activity against multidrug-resistant Pseudomonas aeruginosa at multiple inocula. Antimicrob Agents Chemother 55:5134–5142
Bergen PJ, Li J, Nation RL, Turnidge JD, Coulthard K, Milne RW (2008) Comparison of once-, twice- and thrice-daily dosing of colistin on antibacterial effect and emergence of resistance: studies with Pseudomonas aeruginosa in an in vitro pharmacodynamic model. J Antimicrob Chemother 61:636–642
Bergen PJ, Li J, Rayner CR, Nation RL (2006) Colistin methanesulfonate is an inactive prodrug of colistin against Pseudomonas aeruginosa. Antimicrob Agents Chemother 50:1953–1958
Garonzik SM, Li J, Thamlikitkul V, Paterson DL, Shoham S, Jacob J, Silveira FP, Forrest A, Nation RL (2011) Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob Agents Chemother 55:3284–3294
Zavascki AP, Goldani LZ, Cao GY, Superti SV, Lutz L, Barth AL, Ramos F, Boniatti MM, Nation RL, Li J (2008) Pharmacokinetics of intravenous polymyxin B in critically-ill patients. Clin Infect Dis 47:1298–1304
Li J, Turnidge J, Milne R, Coulthard K (2001) In vitro pharmacodynamic properties of colistin and colistin methanesulfonate against Pseudomonas aeruginosa isolates from patients with cystic fibrosis. Antimicrob Agents Chemother 45:781–785
Velkov T, Roberts KD, Nation RL, Thompson PE, Li J (2013) Pharmacology of polymyxins: new insights into an ‘old’ class of antibiotics. Future Microbiol 8:711–724
Nation RL, Velkov T, Li J (2014) Colistin and Polymyxin B: Peas in a pod, or chalk and cheese? Clin Infect Dis 59:88–94
Cheah SE, Li J, Nation RL, Bulitta JB (2015) Novel rate-area-shape modeling approach to quantify bacterial killing and regrowth for in vitro static time-kill studies. Antimicrob Agents Chemother 59:381–388
Clausell A, Garcia-Subirats M, Pujol M, Busquets MA, Rabanal F, Cajal Y (2007) Gram-negative outer and inner membrane models: insertion of cyclic cationic lipopeptides. J Phys Chem B 111:551–563
Helander IM, Kilpelainen I, Vaara M (1994) Increased substitution of phosphate groups in lipopolysaccharides and lipid A of the polymyxin-resistant pmrA mutants of Salmonella typhimurium: a 31P-NMR study. Mol Microbiol 11:481–487
Moskowitz SM, Ernst RK, Miller SI (2004) PmrAB, a two-component regulatory system of Pseudomonas aeruginosa that modulates resistance to cationic antimicrobial peptides and addition of aminoarabinose to lipid A. J Bacteriol 186:575–579
Helander IM, Kato Y, Kilpeläinen I, Kostiainen R, Lindner B, Nummila K, Sugiyama T, Yokochi T (1996) Characterization of lipopolysaccharides of polymyxin-resistant and polymyxin-sensitive Klebsiella pneumoniae O3. Eur J Biochem 237:272–278
Clements A, Tull D, Jenney AW, Farn JL, Kim SH, Bishop RE, McPhee JB, Hancock RE, Hartland EL, Pearse MJ, Wijburg OL, Jackson DC, McConville MJ, Strugnell RA (2007) Secondary acylation of Klebsiella pneumoniae lipopolysaccharide contributes to sensitivity to antibacterial peptides. J Biol Chem 282:15569–15577
Perez JC, Groisman EA (2007) Acid pH activation of the PmrA/PmrB two-component regulatory system of Salmonella enterica. Mol Microbiol 63:283–293
Adams MD, Nickel GC, Bajaksouzian S, Lavender H, Murthy AR, Jacobs MR, Bonomo RA (2009) Resistance to colistin in Acinetobacter baumannii associated with mutations in the PmrAB two-component system. Antimicrob Agents Chemother 53:3628–3634
Beceiro A, Llobet E, Aranda J, Bengoechea JA, Doumith M, Hornsey M, Dhanji H, Chart H, Bou G, Livermore DM, Woodford N (2011) Phosphoethanolamine modification of lipid A in colistin-resistant variants of Acinetobacter baumannii mediated by the pmrAB two-component regulatory system. Antimicrob Agents Chemother 55:3370–3379
Fernandez L, Gooderham WJ, Bains M, McPhee JB, Wiegand I, Hancock RE (2010) Adaptive resistance to the “last hope” antibiotics polymyxin B and colistin in Pseudomonas aeruginosa is mediated by the novel two-component regulatory system ParR-ParS. Antimicrob Agents Chemother 54:3372–3382
Velkov T, Thompson PE, Nation RL, Li J (2010) Structure-activity relationships of polymyxin antibiotics. J Med Chem 53:1898–1916
Weinstein J, Afonso A, Moss E Jr, Miller GH (1998) Selective chemical modifications of polymyxin B. Bioorg Med Chem Lett 8:3391–3396
Tsubery H, Ofek I, Cohen S, Fridkin M (2001) N-terminal modifications of Polymyxin B nonapeptide and their effect on antibacterial activity. Peptides 22:1675–1681
Tsubery H, Ofek I, Cohen S, Fridkin M (2000) Structure-function studies of polymyxin B nonapeptide: implications to sensitization of gram-negative bacteria. J Med Chem 43:3085–3092
Vaara M, Fox J, Loidl G, Siikanen O, Apajalahti J, Hansen F, Frimodt-Møller N, Nagai J, Takano M, Vaara T (2008) Novel polymyxin derivatives carrying only three positive charges are effective antibacterial agents. Antimicrob Agents Chemother 52:3229–3236
O'Dowd H, Kim B, Margolis P, Wang W, Wu C, Lopez SL, Blais J (2007) Preparation of tetra-Boc-protected polymyxin B nonapeptide. Tetrahedron Lett 48:2003–2005
Chihara S, Ito A, Yahata M, Tobita T, Koyama Y (1974) Chemical synthesis, isolation, and characterization of alpha-N-fattyacyl colistin nonapeptide with special reference to the correlation between antimicrobial activity and carbon number of fattyacyl moiety. Agr Biol Chem 38:521–529
Leese RA (2010) Antibiotic compositions for the treatment of Gram-negative infections. US Patent Number 8343912
Velkov T, Roberts KD, Nation RL, Wang J, Thompson PE, Li J (2014) Teaching ‘old’ polymyxins new tricks: new-generation lipopeptides targeting gram-negative superbugs. ACS Chem Biol 9:1172–1177
Srimal S, Surolia N, Balasubramanian S, Surolia A (1996) Titration calorimetric studies to elucidate the specificity of the interactions of polymyxin B with lipopolysaccharides and lipid A. Biochem J 315(Pt 2):679–686
Soon RL, Velkov T, Chiu F, Thompson PE, Kancharla R, Roberts K, Larson I, Nation RL, Li J (2011) Design, synthesis, and evaluation of a new fluorescent probe for measuring polymyxin-lipopolysaccharide binding interactions. Anal Biochem 409:273–283
Zhao J, Cheah S-E, Roberts KD, Nation RL, Thompson PE, Velkov T, Du Z, Johnson MD, Li J (2016) Transcriptomic Analysis of the Activity of a Novel Polymyxin against Staphylococcus aureus. mSphere 1(4):e00119-16
Bonomo RA, Van Zile PS, Li Q, Shermock KM, McCormick WG, Kohut B (2007) Topical triple-antibiotic ointment as a novel therapeutic choice in wound management and infection prevention: a practical perspective. Expert Rev Anti-Infect Ther 5:773–782
Zhu C, Zhao J, Kempe K, Wilson P, Wang J, Velkov T, Li J, Davis TP, Whittaker MR, Haddleton DM (2017) A hydrogel-based localized release of colistin for antimicrobial treatment of burn wound infection. Macromol Biosci 17(2):1600320
Steinstraesser L, Trust G, Rittig A, Hirsch T, Kesting MR, Steinau HU, Jacobsen F (2011) Colistin-loaded silk membranes against wound infection with Pseudomonas aeruginosa. Plast Reconstr Surg 127:1838–1846
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Velkov, T., Zhu, C., Haddleton, D.M., Li, J. (2017). Novel Antimicrobial Peptides: Targeting Wound Infections Caused by ‘Superbugs’ Resistant to All Current Antibiotics. In: Shiffman, M., Low, M. (eds) Burns, Infections and Wound Management. Recent Clinical Techniques, Results, and Research in Wounds, vol 2. Springer, Cham. https://doi.org/10.1007/15695_2017_34
Download citation
DOI: https://doi.org/10.1007/15695_2017_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-10685-0
Online ISBN: 978-3-030-10686-7
eBook Packages: MedicineMedicine (R0)