Abstract
Prior epidemiologic studies have shown that increasing body mass index (BMI) is associated with higher total cholesterol and low-density lipoprotein cholesterol (LDL). However, these studies were limited by underrepresentation of obese subjects. The aim of this study was to determine whether there is an association between BMI and lipid profiles in a population of patients with a broad spectrum of BMI values. A case-control study was performed involving patients seen at the Cleveland Clinic Florida. Cases (BMI >30 kg/m2) were obtained from the obesity surgery database between August 31, 2000, and April 4, 2002. Controls (BMI ≤ 30 kg/m2) were obtained from a database of primary care physicians between May 1, 2004, and November 18, 2004. Pearson correlation coefficients were used to assess the relationship between BMI and lipid fractions. Multiple linear regression was performed to assess the independent effect of BMI on lipid levels while adjusting for potential confounders and propensity scores. Six hundred thirty-seven patients were analyzed (females, n = 362, 57%). There was no association between higher BMI and LDL (r = 0.19 p = 0.07), a negative association with high-density lipoprotein cholesterol (HDL; r = 0.45, p < 0.001), and a positive association with the log transformation of triglycerides (r = 0.32, p = 0.005).
Higher BMI was inversely associated with HDL and directly associated with TG. BMI showed no significant association with LDL. Although the association between BMI and both HDL and TG may be explained by insulin resistance, the lack of a significant association between BMI and LDL remains an unexpected finding that requires further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Numerous epidemiologic studies have demonstrated a direct correlation between increasing body mass index (BMI) and elevated total cholesterol (TC), low-density lipoprotein cholesterol (LDL), and triglycerides (TG) and an inverse relationship with high density lipoprotein cholesterol (HDL) [1–3]. This association between BMI and lipoprotein levels, particularly LDL, has been suggested to be a contributing factor in the higher rates of cardiovascular events associated with obesity. However, the underrepresentation of individuals with obesity and especially morbid obesity in these studies limits conclusions with regard to expected lipid profiles in this subgroup.
Recently, observational studies of obese patients have confirmed a correlation between BMI and TG or HDL, but not with LDL levels [4]. These findings have raised the question of a possible “obesity paradox” where LDL levels may plateau or even fall with extreme levels of BMI [5, 6]. Therefore, we sought to study the association between BMI and lipoprotein levels in a population with a wide range of BMI subjects including some with morbid obesity.
Methods
Study Population
A retrospective case-control study of patients seen at the Cleveland Clinic Florida was performed. The study was approved by the Institutional Review Board. Consecutive obese patients (cases) were obtained from the obesity surgery database between August 31, 2000, and April 4, 2002. Obesity was defined as a BMI ≥ 30 kg/m2. Consecutive nonobese patients (controls) were obtained from a database of primary care physicians between May 1, 2004, and November 17, 2004.
Data Collection
Patient demographics and medical data were collected from an electronic medical record including the following: age, gender, height, weight, BMI, waist size, menopausal status, current tobacco use, history of diabetes, hypertension, coronary artery disease (CAD), myocardial infarction, and use of hormone replacement therapy, insulin, statin, or other cholesterol-lowering medication. Laboratory tests included a standard fasting lipid profile with TC, LDL, HDL, and TG.
Statistical Analysis
Descriptive analysis for categorical variables with frequency, percentage, and comparisons using chi-square tests were performed. Continuous variables were described as a mean ± standard deviation (SD) and compared by using t tests.
Primary outcomes were TC, LDL, HDL, and TG as continuous variables. For TG, a log-transformed outcome was created because this variable did not have a normal distribution. Pearson coefficients evaluated the correlation between continuous BMI with each of the above-described outcomes. Multivariable linear analysis was performed to evaluate the relation between BMI and each of the lipid measurements while adjusting for potential confounders (age, gender, diabetes, hypertension, current smoking, history of CAD, and statin use).
To further adjust for the potential selection bias when choosing cases and controls, we calculated the probability or propensity score to be a case or a control per patient. The closer the propensity score is to 1, the higher the probability to be a case. The propensity scores were derived from a logistic regression model that included case or control as the outcome and several independent variables (BMI, age, gender, current smoking, history of diabetes, hypertension, CAD, and statin use). We included the propensity scores in all multivariable linear regression analyses. We finally explored the association between BMI and lipids in men and women and in patients with and without use of statins. A p < 0.05 was considered statistically significant. Analyses were performed using SPSS 11.0 and S-Plus 6.1 software packages.
Results
Six hundred thirty-seven patients (female, 67%) were studied. Tables 1 and 2 show the distribution of patient characteristics and cholesterol profiles by BMI levels. The case group is younger with a higher prevalence of female gender and diabetes, whereas the control group has a higher prevalence of CAD and statin use. For the overall population, there was no association between BMI and TC (Pearson correlation coefficient = 0.002, p = 0.96) or LDL (correlation coefficient = 0.078, p = 0.06). There was an association between BMI and HDL (correlation coefficient = -0.267, p < 0.001) and log of TG (correlation coefficient = 0.163, p = 0.006).
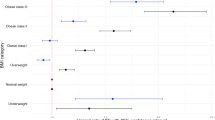
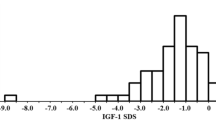
Multivariable linear analysis while adjusting for confounders and propensity scores confirmed a statistically significant association between BMI and both HDL and TG (Tables 3 and 4). HDL was also associated with age, gender, and use of statins, whereas TG was associated with history of hypertension, smoking, and use of statins. There was a 0.25 mg/dL decline in HDL per each unit of increase of BMI and a 1 mg/dL per unit increase in TG per unit increase in BMI. The association between BMI and HDL was significant in women only, after adjusting for covariates (p < 0.01; Fig. 1a). Similarly, the association between BMI and TG was significant in women only (p < 0.001; Fig. 1b). LDL levels were not associated with BMI even after adjustment for confounders and propensity scores (Table 5, Fig. 1c and Fig. 2).
Discussion
In a broad range of BMI patients including the morbidly obese, we found a strong positive association between BMI and TG and a significant inverse association with HDL. However, there was a lack of association of BMI to LDL and TC. The lack of a correlation between BMI and LDL in a broad range of BMI patients is in contrast to findings derived from epidemiologic studies that did not include a high proportion of patients with high BMI.
The Framingham study and other large epidemiologic studies have reported a correlation between obesity and increased coronary heart disease-related events [7–9]. The proposed mechanisms for cardiac events in obese patients include increased atherosclerosis related to dyslipidemia, [10] insulin resistance, hypertension, and diabetes [11, 12].The effects of dyslipidemia on cardiac events is generally considered to be largely due to increased TC [13] and LDL cholesterol [14–20]. However, recent data have suggested that this paradigm of a direct correlation between BMI and LDL cholesterol may be oversimplified. In fact, an “obesity paradox” has been suggested with a weaker than expected correlation between LDL and BMI [21 – 26]. In the NHANES III, the cohort with the highest BMI of ≥ 35 kg/m2 had a lower prevalence of hyperlipidemia (TC >240 or self-reported hyperlipidemia) than the three cohorts with lower BMI. A study by Drapeau et al. found that the extremely (BMI >61 kg/m2) and severely (BMI >46 and <60 kg/m2) obese had a better LDL than the moderately obese (BMI >31-45 kg/m2), whereas the HDL mean level did not deteriorate linearly once the obesity BMI threshold (BMI 30 kg/m2) was passed [6].
Some investigators have suggested that LDL particle size but not its level may be a more important determinant of atherogenicity. Small experimental studies have found that changes in metabolic conditions such as obesity affect predominantly LDL particle size more so than LDL absolute levels [6, 27]. Rainwater et al. showed that a BMI >29.2 kg/m2 is inversely and significantly correlated to LDL particle size (r = -0.128). Particle size is affected by insulin resistance, which is largely due to obesity [28–30]. This change in particle size was shown to result in a greater atherogenic milieu independent of LDL level.
The limitations to our study should be noted. This is a retrospective study of modest size deriving obese patients selected for consideration for obesity surgery. The size of the study is significantly smaller than epidemiologic studies. A small correlation between BMI and LDL may have been evident in a larger sample size. Most variables that affect LDL levels were accounted for in our analysis, although the study was underpowered to determine if the association is present in subgroups of patients. Similar to most studies of patients undergoing obesity surgery, the patient population was predominantly young premenopausal females.
In summary, the common belief that increasing BMI results in a substantially higher TC and LDL may not extend to morbidly obese patients. It is clear that the effect of obesity on insulin resistance results in an increase in TG and a lowering of HDL; however, the effect on LDL level and particle size is not well established. Further study is warranted to evaluate this correlation between obesity and lipid particles.
References
Krauss RM, Winston M, Fletcher BJ, et al. Obesity: impact on cardiovascular disease. Circulation. 1998;98:1472–6.
Després JP, Moorjani S, Tremblay A, et al. Relation of high plasma triglyceride levels associated with obesity and regional adipose tissue distribution to plasma lipoprotein–lipid composition in premenopausal women. Clin Invest Med. 1989;12:374–80.
Denke MA, Sempos CT, Grundy SM. Excess body weight. An under-recognized contributor to dyslipidemia in white American women. Arch Intern Med. 1994;154:401–10.
Nicholls SJ, Tuzcu EM, Sipahi I, et al. Effects of obesity on lipid-lowering, anti-inflammatory, and antiatherosclerotic benefits of atorvastatin or pravastatin in patients with coronary artery disease (from the REVERSAL Study). Am J Cardiol. 2006;97:1553–7.
McTigue K, Larson JC, Valoski A, et al. Mortality and cardiac and vascular outcomes in extremely obese women. JAMA. 2006;296:79–86.
Drapeau V, Lemieux I, Richard D, et al. Metabolic profile in severely obese women is less deteriorated than expected when compared to moderately obese women. Obes Surg. 2006;16:501–9.
Anderson KM, Wilson PW, Garrison RJ, et al. Longitudinal and secular trends in lipoprotein cholesterol measurements in a general population sample. The Framingham Offspring Study. Atherosclerosis. 1987;68:59–66.
Newman B, Selby JV, Quesenberry CP, et al. Nongenetic influences of obesity on other cardiovascular disease risk factors: an analysis of identical twins. Am J Public Health. 1990;80:675–8.
Bertsias G, Mammas I, Linardakis M, et al. Overweight and obesity in relation to cardiovascular disease risk factors among medical students in Crete, Greece. BMC Public Health. 2003;3–3.
Kannel WB, Lebauer EJ, Dawber TR, et al. Relation of body weight to development of coronary heart disease: the Framingham Study. Circulation. 1967;35:734–44.
Howard BV, Knowler WC, Vasquez B, et al. Plasma and lipoprotein cholesterol and triglyceride in the Pima Indian population. Comparison of diabetics and nondiabetics. Arteriosclerosis. 1984;4:462–71.
Uusitupa M, Siitonen O, Voutilainen E, et al. Serum lipids and lipoproteins in newly diagnosed non-insulin-dependent (type II) diabetic patients, with special reference to factors influencing HDL-cholesterol and triglyceride levels. Diab Care. 1986;9:17–22.
Jousilahti P, Tuomilehto J, Vartiainen E, et al. Body Weight, Cardiovascular risk factors, and coronary mortality. 15-Year follow-up of middle-aged men and women in eastern Finland. Circulation. 1996;93:1372–9.
Reeder BA, Angel A, Ledoux M, et al. Obesity and its relation to cardiovascular disease risk factors in Canadian adults. Canadian Heart Health Surveys Research Group CMAJ. 1992;146:2009–19.
Rifkind BM, Begg T, Jackson ID. Relationship of plasma lipids and lipoproteins to obesity. Proc R Soc Med. 1966;59:1277–8.
Angel A. Pathophysiologic changes in obesity. CMAJ. 2005;23:421–9.
Williams PT, Krauss RM. Associations of age, adiposity, menopause, and alcohol intake with low-density lipoprotein subclasses arteriosclerosis, thrombosis, and vascular biology. Arterioscler Thromb Vasc Biol 1997;17:1082–90.
Panagiotakos DB, Pitsavos C, Chrysohoou C, et al. Epidemiology of overweight and obesity in a Greek adult population: the ATTICA Study. Obes Res. 2004;12:1914–20.
Denke MA, Sempos CT, Grundy SM. Excess body weight. An underrecognized contributor to high blood cholesterol levels in white American men. Arch of Int Med. 1993;153:1093–103.
Carroll MD, Lacher DA, Sorlie PD, et al. Trends in serum lipids and lipoproteins of adults, 1960-2002. JAMA. 2005;294:1773–81.
Onat A, Hergenc G, Sari I, et al. Elevated LDL-cholesterol level predicts diabetes in centrally obese women but not men: relative roles of insulin resistance and central obesity. Circ J. 2007;71:1463–7.
Hershcopf RJ, Elahi D, Andres R, et al. Longitudinal changes in serum cholesterol in man: an epidemiologic search for an etiology. J Chron Dis. 1982;35:101–14.
Carr MC, Brunzell JD. Abdominal obesity and dyslipidemia in the metabolic syndrome: importance of type 2 diabetes and familial combined hyperlipidemia in coronary artery disease risk. J Clin Endocrinol Metab. 2004;89:2601–7.
Weinbrenner T, Schröder H, Escurriol V, et al. Circulating oxidized LDL is associated with increased waist circumference independent of body mass index in men and women. Am J Clin Nutr. 2006;83:30–5.
Dixon JB, O'Brien P. A disparity between conventional lipid and insulin resistance markers at body mass index levels greater than 34 kg/m(2). Int J Obes Relat Metab Disord. 2001;25:793–7.
Vierhapper H, Nardi A, Grösser P. Prevalence of paradoxically normal serum cholesterol in morbidly obese women. Metabolism. 2000;49:607–10.
Rainwater DL, Mitchell BD, Comuzzie AG, Haffner SM. Relationship of low-density lipoprotein particle size and measures of adiposity. Int J Obes Relat Metab Disord. 1999;23:180–9.
Barakat HA, Carpenter JW, McLendon VD, et al. Influence of obesity, impaired glucose tolerance, and NIDDM on LDL structure and composition. Possible link between hyperinsulinemia and atherosclerosis. Diabetes. 1990;39:1527–33.
Goff DC, D'Agostino RB, Haffner SM, et al. Insulin resistance and adiposity influence lipoprotein size and subclass concentrations. Results from the Insulin Resistance Atherosclerosis Study. Metabolism. 2005;54:264–70.
Saroja VV, Guowen C, Shelley CA, et al. Common set of genes regulates low-density lipoprotein size and obesity-related factors in Alaskan Eskimos: results from the GOCADAN study. Am J Hum Biol. 2006;18:525–31.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Author Disclosures
Dr. Samuel Szomstein is Consultant for Ethicon Endosurgery and for Covidien
Dr. Raul J Rosenthal is Ethicon Consultant and Educational Grant
Covidien Consultant and Educational Grant
Storz Consultant and Educational grant
Synovis Consultant and Educational
Rights and permissions
About this article
Cite this article
Shamai, L., Lurix, E., Shen, M. et al. Association of Body Mass Index and Lipid Profiles: Evaluation of a Broad Spectrum of Body Mass Index Patients Including the Morbidly Obese. OBES SURG 21, 42–47 (2011). https://doi.org/10.1007/s11695-010-0170-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0170-7