Abstract
Purpose
To assess the incidence, prognostic factors, and clinical outcomes of hepatic encephalopathy (HE) after transjugular intrahepatic portosystemic shunt (TIPS) creation.
Materials and Methods
In this single-institution retrospective study, 191 patients (m:f = 114:77, median age 54 years, median Model for End-Stage Liver Disease or MELD score 14) who underwent TIPS creation between 1999 and 2013 were studied. Medical record review was used to identify demographic characteristics, liver disease, procedure, and outcome data. Post-TIPS HE within 30 days was defined by new mental status changes and was graded according to the West Haven classification system. The influence of data parameters on HE occurrence and 90-day mortality was assessed using binary logistic regression.
Results
TIPS was successfully created with hemodynamic success in 99 % of cases. Median final PSG was 7 mmHg. HE incidence within 30 days was 42 % (81/191; 22 % de novo, 12 % stable, and 8 % worsening). Degrees of HE included grade 1 (46 %), grade 2 (29 %), grade 3 (18 %), and grade 4 (7 %). Medical therapy typically addressed HE, and shunt reduction was necessary in only three cases. MELD score (P = 0.020) and age (P = 0.009) were significantly associated with HE development on multivariate analysis. Occurrence of de novo HE post-TIPS did not associate with 90-day mortality (P = 0.400), in contrast to worsening HE (P < 0.001).
Conclusions
The incidence of post-TIPS HE is non-trivial, but symptoms are typically mild and medically managed. HE rates are higher in older patients and those with worse liver function and should be contemplated when counseling on expected TIPS outcomes and post-procedure course.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatic encephalopathy (HE) is a well-known progressive neural disorder associated with hepatic insufficiency [1]. The mechanism of HE is complex, involving overproduction of enteric neurotoxins from intestinal microflora, reduced hepatic filtering due to liver dysfunction or vascular shunting from the portal to systemic circulations, and increased permeability of the blood–brain barrier [2, 3]. Effects range from mild behavioral change with shortened attention, confusion, and somnolence to coma and death [3]. HE occurs frequently after transjugular intrahepatic portosystemic shunt (TIPS) procedures and represents an important drawback of this otherwise valuable and life-prolonging intervention, which has shown survival benefit in the setting of both refractory variceal hemorrhage and intractable ascites [4–6]. The complexity of HE is further demonstrated by inconsistent clinical data regarding post-TIPS incidence—estimated to range between 22 and 50 %—and associated risk factors [7–11], as well as impact on mortality [12, 13]. As a result, guidelines regarding HE as a contraindication to TIPS are inconsistent [5, 14], and factors influencing patient risk stratification are unclear. Therefore, although post-TIPS HE has been explored in several large studies [8, 11, 15], the present investigation was undertaken with the purpose of providing a detailed and contemporary assessment of the incidence, prognostic factors, and clinical outcomes of HE after TIPS creation in a large cohort of consecutive patients at a single institution over a 13-year period.
Materials and Methods
Institutional review board approval was granted for this study with waiver of consent for inclusion. Patients provided written informed consent for TIPS procedures.
Study Population
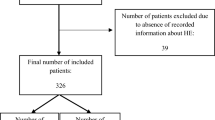
Electronic medical records for 270 consecutive patients who underwent technically successful TIPS procedures between November 1999 and April 2013 at a tertiary care, academic university-affiliated hospital were identified through review of the Division of Interventional Radiology (IR) TIPS registry and were selected for possible retrospective study. Patients were excluded for inadequate 30-day clinical follow-up, including 10 patients who underwent early liver transplantation, 43 patients who expired, and an additional 26 patients without sufficiently documented clinical assessment. Of the 43 patients excluded for 30-day mortality (mean survival time 9 days), the most common causes of death were related to hemorrhage (n = 16), liver failure (n = 9), or spontaneous bacterial peritonitis (SBP) with sepsis (n = 6). The final study cohort thus comprised 191 patients.
Procedure Indications and TIPS Protocol
TIPS creation was performed according to conventional methods [16] for customary indications, including variceal hemorrhage and medically refractory ascites. Venous access was gained through the right jugular vein. Catheter access into the right hepatic vein allowed performance of free and wedged hepatic venography as well as intravascular pressure measurement. A Rösch–Uchida transjugular liver access set (Cook Medical Co., Bloomington, IN, USA) was used to penetrate the liver for access to the right portal vein. Catheterization, pressure measurement, and balloon dilation of the hepatic parenchymal tract were performed, followed by deployment of a 10- to 12-mm Wallstent bare metal stent (Boston Scientific, Natick, MA, USA) (used from 2000 to 2003) or 10-mm Viatorr covered stent graft (W. L. Gore & Associates, Flagstaff AZ) (used from 2004 to 2013) across the liver tract. Balloon dilation was performed using a 7- to 10-mm balloon, followed by shunt venography. Coil embolization of gastroesophageal varices was performed at the discretion of the primary operator. Following TIPS procedures, patients underwent inpatient monitoring for 48–72 h and were then followed in an outpatient hepatology clinic.
Measured Outcomes
Measured outcomes included first occurrence of HE within 30 days of TIPS procedures, associated factors, and impact on survival. HE was defined as alteration in central nervous system function due to hepatic insufficiency, as determined clinically by the patient’s hepatologist. The presence or the absence of HE, which was determined subjectively by the patient’s hepatologist, was consistently noted in the medical record and was used to identify patients who had post-TIPS HE. However, the severity of HE was not routinely noted in the medical record, and the determination of HE grade was made as diligently as possible during data collection according to the West Haven classification system (Table 1) [1, 3]. The 30-day time interval was selected because previous reports demonstrate that HE most frequently develops within this post-TIPS time period [15, 17] and because procedure-related adverse events are routinely reported within the 30-day time frame [18].
All patient records were evaluated for occurrence of HE post-TIPS, grade of HE, and time-to-event. De novo HE referred to the subset of all post-TIPS HE patients who had no prior history of clinically significant HE, whereas worsened HE referred to the subset with post-TIPS HE at least one grade worse than all prior events. A patient with a history of HE without any HE manifestations at the time of TIPS and who developed HE after TIPS was not considered to have worsened HE unless HE grade post-TIPS exceeded the historical HE grade pre-TIPS. Data acquired for associated factors included use of empiric treatment (preemptive peri-procedural HE medical therapy using lactulose, rifaximin, or metronidazole in patients with no HE history), serum ammonia levels within 7 days prior to TIPS, previous history of SBP, total liver volume (quantified using computed tomography or magnetic resonance imaging volumetric analysis), previous HE history, presence or absence of HE at the time of TIPS (immediate pre-intubation data were utilized to assess HE status in intubated patients), and pre- and post-TIPS HE medications. After initiation of HE therapy, the effectiveness of HE treatment was based on hepatologist documentation in the medical record of HE symptom persistence or resolution.
Other outcome measures included TIPS technical results and 90-day overall patient survival. TIPS hemodynamic success was defined as reduction in the portosystemic pressure gradient (PSG) to an absolute value ≤12 mmHg [5, 14].
Statistical Analysis
Patient characteristics were reported using descriptive statistics as number (percent) or median (interquartile range). Comparisons for categorical data were performed using the Pearson’s chi-squared test or Fisher’s exact test. Comparisons for continuous nonparametric non-paired data sets were performed using the Wilcoxon’s rank-sum test. Multivariate binary logistic regression analysis was used to assess the influence of demographic and anatomic factors, liver disease scores, laboratory and clinical findings, and procedure parameters on 30-day HE outcomes. For the purposes of multivariate analysis, laboratory parameters comprising the Child–Pugh and Model for End-Stage Liver Disease (MELD) scores were not entered into the model if these scores were inputted in order to avert multicollinearity phenomenon. Statistical analysis was performed with SPSS, version 21 (SPSS Inc., Chicago, IL, USA). P values ≤0.05 were considered statistically significant.
Results
Patients and TIPS Procedures
Patient demographics and liver disease characteristics are summarized in Table 2. The majority of patients (94/191, 49 %) received TIPS due to variceal bleeding, which was confirmed with upper endoscopy. Patients with recurrent or refractory ascites and hepatic hydrothorax (92/191, 48 %) had failed prior conventional treatment, including dietary sodium and fluid restriction as well as diuretic therapy. Five patients (3 %) with portal vein thrombus underwent TIPS to prevent clot propagation in order to maintain liver transplant candidacy. Thirty-eight of 191 (20 %) procedures were urgent in nature.
TIPS hemodynamic success was achieved in 189/191 (99 %) patients. Covered stent grafts were used in 160/191 (84 %) cases, and variceal embolization was performed in 38/191 (20 %) procedures. Median pre- and post-TIPS PSGs were 20 (range 16–24) and 7 (range 5–9) mmHg, respectively. Median PSG reduction was 13 (range 10–16) mmHg. Regarding procedure-related complications, two patients (1 %) had ischemic hepatitis within 30 days, defined by marked transient elevation in liver transaminase levels, which recovered spontaneously within a few weeks.
HE Incidence
Encephalopathy data are summarized in Table 3. The cumulative incidence of HE within 30 days of TIPS was 42 % (81/191). Twenty-two percent of patients had de novo HE, 8 % had worsening HE, and the remaining 12 % had stable HE. Median time to the first HE episode was 19 days; however, the worsening HE cohort developed HE sooner, at approximately 14 days post-TIPS, but this was not statistically different from de novo cases (P = 0.237). HE grades were primarily mild (grade 1, 46 %) or moderate (grade 2, 29 %).
Of the entire cohort, 91/191 (48 %) patients had prior HE, but of these, only 39/91 (43 %) went on to develop HE post-TIPS. Among the 91 patients with a pre-TIPS history of HE, 28 (31 %) were grade 1, 12 (13 %) were grade 2, 11 (12 %) were grade 3, and 4 (4 %) were grade 4. Thirty-six of 91 (40 %) patients did not have enough clinical information in the electronic medical record to ascertain pre-TIPS HE grade. Prior to TIPS, 54/91 (59 %) patients with an HE history had been treated with lactulose alone, while only 5 (5.5 %) were treated with lactulose and rifaximin. The remaining patients were treated with lactulose and metronidazole (n = 6, 6.5 %), metronidazole alone (n = 1, 1 %), neomycin alone (n = 1, 1 %), rifaximin alone (n = 8, 9 %), or no medications (n = 16, 18 %). Twenty-four of 54 (44 %) patients treated with lactulose developed HE within 30 days of TIPS, while 2/5 (40 %) patients treated with lactulose and rifaximin developed HE within 30 days of TIPS; the incidence of post-TIPS HE was not statistically different between these groups (P > 0.999).
Most patients with prior history of HE (85/91, 93 %) received HE pharmacologic therapy at the time of TIPS, compared to only 20/100 (20 %) of those without prior history of HE who received empiric therapy. Of the 85 patients with a history of HE prior to TIPS and on medical therapy, 76 (89.5 %) had no HE manifestations at the time of TIPS, 8 (9.5 %) manifested some HE symptomatology at the time of TIPS, and 1 (1 %) was intubated but had not pre-intubation HE symptoms. Thirty-seven (44 %) of these patients went on to have post-TIPS HE. Thirty-three of 37 (89 %) had no HE manifestations at the time of TIPS, while 4/37 (11 %) had some HE symptoms at the time of TIPS. Among these four patients, HE grades were 2, 2, 3, and 4 pre-TIPS and 1, 2, 3, and 4 post-TIPS (all stable HE).
Baseline ammonia levels were overall higher in patients who developed de novo HE and lower in patients who developed worsening HE (median 133 vs. 92 μg/dL), though data were limited by small patient number and were not statistically significant (P = 0.521).
Risk Factors for HE
Results of univariate and multivariate analysis of parameters associated with HE are presented in Table 4. MELD score >18 (58 vs. 37 %, P = 0.009) and patient age >65 (62 vs. 39 %, P = 0.020) were independently associated with occurrence of HE on multivariate regression. New or worsening HE was associated with age >65 (P = 0.023), female gender (P = 0.015), and small liver volume (P = 0.049) on univariate analysis, but was not confirmed on multivariate analysis. No other measure showed association with HE post-TIPS.
Of note, there was no threshold PSG that predisposed patients to greater HE risk. HE incidence was similar for patients with a final PSG ≤5 versus >5 mmHg (21/50, 42 % vs. 59/139, 42 %; P = 0.956) and a final PSG ≤8 versus >8 mmHg (55/134, 41 % vs. 25/55, 46 %; 0.577). Additionally, there was no threshold bilirubin level that inclined patients to greater HE risk. HE incidence was similar for patients with a baseline bilirubin level <2.0 versus ≥2.0 mg/dL (54/125, 43 % vs. 27/66, 41 %; P = 0.761).
HE Treatment
Among the 81 patients who had post-TIPS HE, 70 (86.5 %) were treated with lactulose, 6 (7.5 %) received lactulose and rifaximin, 2 (2.5 %) were managed with lactulose and metronidazole, 1 (1 %) was given only metronidazole, and 2 (2.5 %) were provided no medications. Among the 16 patients with worsening HE post-TIPS, 10 (62.5 %) had been treated with lactulose pre-TIPS, 2 (12.5 %) received lactulose and rifaximin before TIPS, and 4 (25 %) were on no medications prior to TIPS. Following TIPS, 13 (81 %) were treated with lactulose and 3 (19 %) received lactulose and rifaximin.
TIPS Reduction or Occlusion
Patients with refractory or persistent HE despite medical therapy were referred for TIPS reduction, which was performed in 3/81 (4 %) patients. Only one of the three patients had a history of pre-TIPS HE (grade 2), which was successfully controlled with both lactulose and rifaximin; none of the patients had HE at the time of TIPS. All the three patients had undergone 10-mm Viatorr covered stent graft TIPS, with a mean PSG reduction of 12 mmHg (from 19 mmHg pre-TIPS to 7 mmHg post-TIPS). Among these three patients, all had first occurrence of HE within 3 weeks post-TIPS (on days 4, 11, and 19). The HE grades post-TIPS were 1, 3 (in the patient with history of HE), and 4. Following TIPS, all three patients were treated with lactulose, and one was treated with rifaximin, without success. All three patients underwent technically successful TIPS reduction using the bidirectionally adjustable reduction technique employing parallel stent and stent graft deployment [19] (Fig. 1). Shunt reduction was performed at 16, 36, and 308 days post-TIPS. One patient went on to receive complete TIPS occlusion with a vascular plug due to persistent HE following shunt reduction (shunt reduction performed at post-TIPS day 36, and shunt occlusion performed at post-TIPS day 64). At the time of TIPS reduction, the mean PSG increased by 5 mmHg (from 12 mmHg pre-TIPS to 17 mmHg post-TIPS). All cases of HE improved after reduction or occlusion with return of baseline cognition level—with no HE—as determined by the patient’s hepatologist.
A 66-year-old man with new grade 4 HE following TIPS for medically refractory ascites necessitating shunt reduction 308 days later. Pre-reduction TIPS venogram (a) shows patent shunt (arrows) with little antegrade intrahepatic portal venous filling (arrowheads); PSG measured 11 mmHg. Fluoroscopic image (b) during shunt reduction demonstrates parallel stent (black arrowhead) and covered stent graft (white arrowheads) used for revision. Post-reduction TIPS venogram (c) displays markedly reduced shunt caliber (arrowheads) and improved antegrade intrahepatic portal venous filling (arrows); PSG measured 24 mmHg and HE quickly resolved
HE Impact on Survival
Mortality between 30 and 90 days following TIPS creation was 9 % (18/191). Patients presenting for refractory ascites had 90-day mortality of 12 % (9/78), while patients presenting for variceal hemorrhage had 90-day mortality of 10 % (9/94). Data on the association of post-TIPS HE and 90-day mortality are presented in Table 5. Occurrence of post-TIPS HE was associated with an increased 90-day mortality rate (19 vs. 3 %, P < 0.001). Notably, however, median MELD score was significantly higher in our HE group (15 vs. 13, P = 0.040) and could account for this difference. The association between HE and early mortality remained true for those patients developing worsening HE (P = 0.001), but not for those developing de novo HE (P = 0.400).
Of note, TIPS urgency was not associated with a statistically significant increase in 90-day mortality (4/38, 11 % vs. 14/167, 8 %; P = 0.750) in the current series. However, this is likely an anomalous outcome related to exclusion of patients who did not meet at least 30-day clinical follow-up: 43 patients who expired prior to 30 days were excluded, and 21 (49 %) of these patients represented urgent TIPS.
Discussion
HE is one of the most challenging adverse side effects of the TIPS procedure. Despite its frequency in cirrhotic patients, a clear understanding of its etiology and effect on patient outcome is lacking [2]. While typically attributed solely to portosystemic shunting, post-TIPS HE can be precipitated by abrupt change in portal perfusion, shunt dysfunction, multiple hepatic re-interventions, and recurrent gastrointestinal bleeding or ascites [10, 11, 17, 20], but can be attenuated by growing tolerance to blood ammonia levels [17]. Studies also show that decreased hepatic reserve—measured by liver volume—is associated with poorer post-procedural course and decreased survival [21, 22]. Based upon the heterogeneity of the existing body of the literature regarding the incidence, associated parameters, and impact of HE post-TIPS, additional investigation is needed to further elucidate clinical prognostic factors and consequences of HE post-TIPS.
In the current study, a large cohort of TIPS patients was analyzed for HE within 30 days of TIPS procedures. Comparable to recent reports, overall HE incidence was 42 %, of which only half was de novo. HE developed about 2–3 weeks post-TIPS in de novo cases, but slightly earlier in patients with prior history of HE. Cases were mostly mild or moderate and amenable to medical management. To this end, only 4 % of patients underwent TIPS reduction or occlusion, which successfully controlled recalcitrant HE when necessary. Nearly half of the patients in the study had prior documented HE, most of which were maintained on HE medical therapy prior to TIPS. The rate of HE post-TIPS in this group was similar to that without prior HE, which suggests that patients who are medically managed do not have increased risk of HE post-TIPS compared to those without prior history. While the current study did not perform a one-to-one comparison, the results are in contrast to a previous report, which found that prior HE predicted post-TIPS HE and saw no improvement with prophylactic therapy [23].
In examining factors associated with HE occurrence, only worse liver function and older patient age were connected with HE after TIPS. This result would be expected based on prior knowledge that HE is a progressive illness associated with hepatic dysfunction. While this result is consistent with previous reports, other previously identified associated factors, including prior HE, sodium level, albumin level, Child–Pugh score, and stent type [7–11], were not confirmed in our study. In cases of new or worsening HE, female gender, older patient age, and smaller liver volume were found to be associated factors, although not established on multivariate analysis. While information about the clinical impact of gender association with HE is lacking, smaller liver volume has previously been shown to correlate with degree of cirrhosis and would also intuitively relate with poor post-procedure course [24]; smaller liver volumes certainly predispose post-surgical patients to liver insufficiency [25]. While not statistically significant, the HE group had elevated baseline ammonia and received more bare metal stents.
In our analysis, post-TIPS HE showed an association with 90-day mortality; however, this was true only among patients with worsening HE. Thus, healthier patients without prior HE may not be at increased risk of early mortality. This would suggest that HE might be more of a marker of poor prognosis instead of a cause; those who have suffered HE previously have overall more progressive disease and are at increased risk of early mortality. This is also supported by the finding that MELD score was a strong predictor of post-TIPS HE and knowledge that MELD score is an excellent predictor of early mortality based on numerous prior reports [26–28].
There exists debate whether prior HE should be a major concern when evaluating patients prior to TIPS. Some authorities suggest that TIPS may be contraindicated in patients with prior HE refractory to lactulose, especially in the context of older age, diabetes, or hemodialysis [14]. However, TIPS may be the only suitable option for patients with decompensated liver disease who have failed medical management or may not be candidates for transplantation. Our data, in which less than half of the patients with pre-TIPS HE went on to develop post-TIPS HE, suggest that prior HE history should not constitute an absolute contraindication to TIPS creation. More prospective studies are needed to better understand which patients will benefit most from receiving TIPS.
There are several limitations to this study. Data were collected retrospectively from a single institution and were non-randomized in nature. Patient treatment spanned the course of a decade, for which there may be differences in medical care and reporting. Development of HE was only determined subjectively by the patient’s hepatologist and was limited to information available in patient charts. While the presence or absence of HE was consistently noted in the medical record, charted details of patient history and physical examination were used to grade HE, which was not routinely classified by grade in the medical record; despite the most attentive and meticulous efforts, the grading of HE based on retrospective data is not ideal. Lastly, all-cause mortality was assessed rather than liver-specific mortality.
In summary, new or worsening HE can affect more than one-third of patients undergoing TIPS for palliation of portal hypertensive complications. Patients should be counseled that most cases are mild or moderate, associated with worse liver function and older age, and that refractory cases can be effectively managed with TIPS reduction or occlusion. Early mortality risk is not increased in individuals without prior episodes of HE. Further studies are needed to identify predictors of poor post-procedure course and clinical impact of developing HE after TIPS.
References
Bajaj JS, Wade JB, Sanyal AJ. Spectrum of neurocognitive impairment in cirrhosis: implications for the assessment of hepatic encephalopathy. Hepatology. 2009;50:2014–2021.
Garcovich M, Zocco MA, Roccarina D, Ponziani FR, Gasbarrini A. Prevention and treatment of hepatic encephalopathy: focusing on gut microbiota. World J Gastroenterol. 2012;18:6693–6700.
Blei AT, Cordoba J. Hepatic encephalopathy. Am J Gastroenterol. 2001;96:1968–1976.
Garcia-Pagan JC, Di Pascoli M, Caca K, et al. Use of early-TIPS for high-risk variceal bleeding: results of a post-RCT surveillance study. J Hepatol. 2013;58:45–50.
Boyer TD, Haskal ZJ, American Association for the Study of Liver Disease. The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension: update 2009. Hepatology. 2010;51:306.
Salerno F, Merli M, Riggio O, et al. Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology. 2004;40:629–635.
Peter P, Andrej Z, Katarina SP, Manca G, Pavel S. Hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in patients with recurrent variceal hemorrhage. Gastroenterol Res Pract. 2013. doi:10.1155/2013/398172.
Masson S, Mardini HA, Rose JD, Record CO. Hepatic encephalopathy after transjugular intrahepatic portosystemic shunt insertion: a decade of experience. QJM. 2008;101:493–501.
Riggio O, Angeloni S, Salvatori FM, et al. Incidence, natural history, and risk factors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stent grafts. Am J Gastroenterol. 2008;103:2738–2746.
Bureau C, Pagan JC, Layrargues GP, et al. Patency of stents covered with polytetrafluoroethylene in patients treated by transjugular intrahepatic portosystemic shunts: long-term results of a randomized multicentre study. Liver Int. 2007;27:742–747.
Tripathi D, Ferguson J, Barkell H, et al. Improved clinical outcome with transjugular intrahepatic portosystemic stent-shunt utilizing polytetrafluoroethylene-covered stents. Eur J Gastroenterol Hepatol. 2006;18:225–232.
Mamiya Y, Kanazawa H, Kimura Y, et al. Hepatic encephalopathy after transjugular intrahepatic portosystemic shunt. Hepatol Res. 2004;30:162–168.
Dissanayake O, MacNaughton J, Patch D, Morgan MY. Hepatic encephalopathy is a significant predictor of mortality following tips insertion for refractory ascites. J Hepatol. 2013;58:S420–S421.
Krajina A, Hulek P, Fejfar T, Valek V. Quality improvement guidelines for transjugular intrahepatic portosystemic shunt (TIPS). Cardiovasc Interv Radiol. 2012;35:1295–1300.
Qin JP, Jiang MD, Tang W, et al. Clinical effects and complications of TIPS for portal hypertension due to cirrhosis: a single center. World J Gastroenterol. 2013;19:8085–8092.
Gaba RC, Omene BO, Podczerwinski ES, et al. TIPS for treatment of variceal hemorrhage: clinical outcomes in 128 patients at a single institution over a 12-year period. J Vasc Interv Radiol. 2012;23:227–235.
Nolte W, Wiltfang J, Schindler C, et al. Portosystemic hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in patients with cirrhosis: clinical, laboratory, psychometric, and electroencephalographic investigations. Hepatology. 1998;28:1215–1225.
Haskal ZJ, Rees CR, Ring EJ, Saxon R, Sacks D, Society of Interventional Radiology Technology Assessment Committee. Reporting standards for transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 2003;14:S419–S426.
Sze DY, Hwang GL, Kao JS, et al. Bidirectionally adjustable TIPS reduction by parallel stent and stent-graft deployment. J Vasc Interv Radiol. 2008;19:1653–1658.
Khungar V, Poordad F. Hepatic encephalopathy. Clin Liver Dis. 2012;16:301–320.
Hagan MT, Sayuk GS, Lisker-Melman M, et al. Liver volume in the cirrhotic patient: does size matter? Dig Dis Sci. (Epub ahead of print). doi:10.1007/s10620-014-3038-1.
Zhu JY, Leng XS, Dong N, Qi GY, Du RY. Measurement of liver volume and its clinical significance in cirrhotic portal hypertensive patients. World J Gastroenterol. 1999;5:525–526.
Riggio O, Masini A, Efrati C, et al. Pharmacological prophylaxis of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt: a randomized controlled study. J Hepatol. 2005;42:674–679.
Tong C, Xu X, Liu C, Zhang T, Qu K. Assessment of liver volume variation to evaluate liver function. Front Med. 2012;6:421–427.
May BJ, Talenfeld AD, Madoff DC. Update on portal vein embolization: evidence-based outcomes, controversies, and novel strategies. J Vasc Interv Radiol. 2013;24:241–254.
Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Gastroenterology. 2001;120:A76–A77.
Gaba RC, Couture PM, Bui JT, et al. Prognostic capability of different liver disease scoring systems for prediction of early mortality after transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol. 2013;24:411–420.
Al Sibae MR, Cappell MS. Accuracy of MELD scores in predicting mortality in decompensated cirrhosis from variceal bleeding, hepatorenal syndrome, alcoholic hepatitis, or acute liver failure as well as mortality after non-transplant surgery or TIPS. Dig Dis Sci. 2011;56:977–987.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Casadaban, L.C., Parvinian, A., Minocha, J. et al. Clearing the Confusion over Hepatic Encephalopathy After TIPS Creation: Incidence, Prognostic Factors, and Clinical Outcomes. Dig Dis Sci 60, 1059–1066 (2015). https://doi.org/10.1007/s10620-014-3391-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3391-0