Abstract
Background
Although its theoretical usefulness has been reported, the true value of automatic smoke evacuation system in laparoscopic surgery remains unknown. This is mainly due to the lack of objective evaluation. The purpose of this study was to determine the efficacy of the automatic smoke evacuator in laparoscopic surgery, by real-time objective evaluation system using an industrial smoke-detection device.
Methods
Six pigs were used in this study. Three surgical ports were placed and electrosurgical smoke was generated in a standard fashion, using either a high-frequency electrosurgical unit (HF-ESU) or laparosonic coagulating shears (LCS). The smoke was evacuated immediately in the evacuation group but not in the control nonevacuation group. The laparoscopic field-of-view was subjectively evaluated by ten independent surgeons. The composition of the surgical smoke was analyzed by mass spectrometry. The residual smoke in the abdominal cavity was aspirated manually into a smoke tester, and stains on a filter paper were image captured, digitized, and semiquantified.
Results
Subjective evaluation indicated superior field-of-view in the evacuation group, compared with the control, at 15 s after activation of the HF-ESU (P < 0.05). The smoke comprised various chemical compounds, including known carcinogens. The estimated volume of intra-abdominal residual smoke after activation of HF-ESU was significantly lower in the evacuation group (47.4 ± 16.6) than the control (76.7 ± 2.4, P = 0.0018). Only marginal amount of surgical smoke was detected in both groups after LCS when the tissue pad was free from burnt tissue deposits. However, the amount was significantly lower in the evacuation group (21.3 ± 10.7) than the control (75 ± 39.9, P = 0.044) when the tissue pad contained tissue sludge.
Conclusions
Automatic smoke evacuation provides better field-of-view and reduces the risk of exposure to harmful compounds.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The smoke generated during electrosurgery reduces visibility in laparoscopic surgery and is harmful not only for the patients but also for surgeons and operating room personnel [1]. In fact, some groups have advocated removal of the surgical smoke using a closed circuit, based on their findings of the presence of various potentially harmful substances in the surgical smoke [2, 3]. In daily practice, however, many laparoscopists release the surgical smoke from the abdominal cavity into the room air, by opening the stopcock of the laparoscopic port [3]. Although commercially available, an automatic smoke evacuation system has not been used widely, mainly because of lack of objective evaluation. The purpose of this study was to evaluate the efficacy of a commercially available automatic smoke evacuator in eliminating surgical smoke, including harmful substances, in experimental laparoscopic surgery, using an industrial smoke-testing device.
Materials and methods
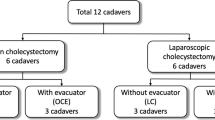
The experimental protocol described in this study was reviewed and approved by the Animal Care and Ethical Review Committee of Osaka University. All animals used in the experiments were sacrificed at the end of the study by deep anesthesia.
Three month-old female, 35-kg domestic swine (LWD swine, n = 6) were fasted overnight before the experiment. Premedication with intramuscular ketamine 10 mg/kg and xylazine 2 mg/kg were administered. After settling in supine position, the animal was intubated and a catheter was cannulated into an ear vein to maintain general anesthesia using 1–3 % isoflurane inhalation. The first trocar for optics was placed midabdomen using open Hasson method, while each of the other two working ports was placed in the lateral abdomen. Carbon dioxide (CO2) pneumoperitoneum was established using a standard automatic CO2 insufflator (UHI-3; Olympus Medical Systems, Tokyo, Japan) with an intra-abdominal pressure of 8 mmHg. Air-tightness was secured by adding a lubricant around each port site. The abdominal cavity was then explored with a rigid-tip, high-definition videolaparoscope (OTV-S7 ProH-HD-12E, Olympus Medical Systems, Tokyo) before the surgical procedures.
The liver surface was exposed laparoscopically and burnt for 30 s to generate smoke in a reproducible fashion, using a laparoscopic hook-shaped electrosurgical probe connected to a high-frequency electrosurgical unit (HF-ESU, VIO300D; ERBE Elektromedizin, Tübingen, Germany) or a laparosonic coagulation shares (LCS, Harmonic®; Ethicon Endo-Surgery, Cincinnati, OH). In the evacuation group, an automatic smoke evacuator (IES2; ERBE), at maximum power (100 %) and delay time of 10 s, equipped with a smoke absorptive membrane (#7-510-16; Northgate Technologies Inc, Scottsdale Court, IL), was connected to one of the working ports via a standard insufflation tube (Fig. 1A). The smoke was simultaneously evacuated while the energy device was activated with the delay time. The absorptive membrane was replaced every two times during the experiment to maintain the maximal absorptive performance of the evacuation system. In the nonevacuation control group, the experiment was repeated without the use of the evacuator (Fig. 1B).
Subjective evaluation of laparoscopic field of view by laparoscopists
Video images of the surgical field were recorded in each group (Movie 1) every 5 s (0–40 s: total 9 images in each group). Each recording was evaluated by ten well-trained surgeons into four grades (excellent, good, fair, and poor surgical view) using appointed questionnaire (Fig. 2A).
Sampling of residual smoke after activation of energy devices
After the activation of energy devices, a smoke tester (Bacharach Smoke Tester, HT-1650; Hodaka, Osaka, Japan) with a dedicated filter paper (HT-1651; Hodaka) was subsequently connected to the working port (Fig. 3A), and the residual smoke in the abdominal cavity was manually aspirated ten times according to the protocol provided by the manufacturer (Movie 2). Stained filter papers (Fig. 3B) were used in the following procedures.
The industrial smoke tester. (a) Filter paper (arrow) was fitted to the cylinder of the smoke tester. (b) The smoke tester equipped with filter paper was connected to the working port. A Collected surgical smoke on the filter papers. B Smoke absorptive membranes used in the smoke evacuation system: (a) before use, (b) after use. C Results of GC–MS analysis (membrane: smoke absorptive membrane). D Peak values are shown at the top of each peak
Component analysis of sampled surgical smoke and membrane
The stained filter paper of each group, the membrane in the closed circuit after use (Fig. 3C, left: before use, right: after use) as a positive control and unstained filter paper as a negative control were cut into small pieces and placed into head space vials, respectively. Vaporization of each sample was performed using TurboMatrix HS40 (Simadzu, Kyoto, Japan) under the following conditions; injection duration: 0.25 min, heat treatment temperature: 120 °C, needle temperature: 120 °C, compression duration: 1 min, incubating duration: 30 min and pressure: 120 kPa. Gas chromatography and mass spectrum (GC–MS) analysis were performed using QP2010 Ultra (Simadzu).
Conversion to carbon concentration of stained filter papers
The stain on the filter paper was digitized (Fig. 4A, top column) using an image scanning device (CanoScan 8800F; Canon, Tokyo). Each image was then converted to a grayscale (Fig. 4A, middle column) using an image retouching software (Photoshop ver. 7; Adobe Systems, San Jose, CA), and semiquantified (Fig. 4A, lower column) using an image analysis software (NIH image ver. 1.63, National Institutes of Health, Washington, D.C.). Conversion to carbon concentration was performed by using a standard scale (RR776, Bacharach, Fig. 4B).
A Semiquantification of surgical smokes collected on the filter papers. Filter papers were image scanned through a common scanning device (top). The scanned stains were converted to a gray scale (middle), and then, semiquantified through Image J software (bottom). B Standard smoke scale supplied with the testing system. C The formula used for conversion of the scored stains to carbon concentration
Real-time objective evaluation of residual smoke after activation of energy devices
HF-ESU challenge
The liver surface was exposed laparoscopically and burnt for 30 s with the HF-ESU. The setting of HF-ESU was splay coagulation mode (Effect: 2 100 W) and 30 s (VIO Time Limit; 30 s). The experiment was repeated twice in each animal of each group, i.e., six times overall in the crossover turn.
LCS challenge
A similar experiment was conducted using LCS instead of the HF-ESU. LCS was applied to the liver edge for 30 s to generate a “mist,” with or without automatic evacuation. The LCS was set at level 5. This protocol was adopted because in daily practice, surgeons frequently encounter further deterioration of laparoscopic vision with the mist, especially when the tissue pad of LCS is covered with sludge. The experiment was accordingly conducted under two different conditions: a clean pad, and a dirty pad with the burnt deposits (Fig. 5B). Because the currently used IES2 is not compatible with the LCS system, the mist was evacuated by activating IES2 with a foot pedal while LCS was activated. The experiment was repeated twice in each animal of each group, i.e., six times overall in the crossover turn. Data of the two groups were compared.
A Semiquantification of carbon concentration in the smoke after HFS-ESU activation. The carbon concentration was significantly lower in the evacuator group than the control (P = 0.0018). B LCS with sludge in the tissue pad. C Semiquantification of carbon concentration after LCS activations under two different conditions. Without burned clot: only a few carbon compounds were detected in both groups; with burned clot: carbon concentration increased in both groups (control: P = 0.0071, evacuator: P = 0.0074). This tendency was intensified in the control group than in evacuator group (P = 0.044)
Statistical analysis
Statistical analyses were performed using JMP 8.0.1 for Windows (SAS Institute, Cary, NC). Possible differences between the two groups in each experiment were analyzed using the Student’s t test, χ 2 test, or Wilcoxon test as appropriate. A probability level of 0.05 was selected to indicate the statistical significance.
Results
Subjective evaluation of the surgical smoke generated by a HF-ESU
Assembling questionnaires described by ten surgeons revealed that the fields of laparoscopic views in the evacuator group were better than those of the control group at 15–40 s after activation of HF-ESU (P < 0.05; Fig. 2B).
Analysis of component included in surgical smoke
The GC–MS analysis identified 42 peaks in the positive control (Fig. 3D) and 37 substances (Table 1). The detected substances were carbon compounds and three were carcinogenic according to the International Agency for Research on Cancer (IRAC) (acetaldehyde: group I; dimethylformamide: group 2B; and furfural: group 3). As shown in Fig. 3D, all peaks on the total ion chromatogram (TIC) of the positive control fitted closely with those of the stained filter paper samples in each group.
Validation of real-time carbon concentration monitoring
To rationalize the scanning devices and NIH software used in this study, we scanned a standard smoke scale pertaining to the testing system (RR776, Bacharach, Inc., New Kensington, PA; Fig. 4B), and converted the obtained images to grayscale images for semiquantification. The scores of the smoke scale correlated linearly and significantly with the grayscale concentration in function (R 2 = 0.992, data not shown). These results confirmed the appropriateness of the current experimental setting. Next, standard smoke scales were beforehand appointed carbon concentrations. We used these standard concentrations to convert the grade of stains on the filter papers to carbon concentrations as follows:
where y is the carbon concentration (mg/m3), and x is the stains converted to standard scores (R 2 = 0.9972).
Real-time objective evaluation of residual smoke after activation of energy devices
HF-ESU challenge
As shown in Fig. 5A, the semiquantified carbon concentration was significantly lower in the evacuator group (0.4 ± 0.27 mg/m3) than the control group (1.7 ± 0.02 mg/m3, P = 0.0018).
LCS challenge
When using LCS with a clean pad, test stains were only marginally detectable and there was no significant difference in the smoke concentration between the two groups (Fig. 5C; evacuator group: 0.002 ± 0.0078 control group: 0.0023 ± 0.0085 mg/m3, P = 0.96). On the other hand, the use of LCS with a sludge in the crotch of the tissue pad significantly lowered the residual smoke concentration (Fig. 5C; evacuator group: 0.018 ± 0.01, control group: 4.4 ± 3.7 mg/m3, P = 0.044).
Discussion
The smoke generated during electrosurgery causes not only surgeon’s stress and prolongation of operating time [4] but also places both patients and operating room personnel at risk of exposure to harmful substances [1, 5–10]. High temperature decomposition generated during tissue ablation is known to produce breathable aerosols, complex organic chemicals, and cellular debris, including carcinogenic substances [4]. The composition of the surgical smoke includes various chemicals, such as aldehydes, benzene, toluene, acrolein, hydrocyanic gases, and carbon monoxide [6, 8, 11–13]. Therefore, the smoke generated by tissue decomposition is presumably cytotoxic, genotoxic, mutagenic, and clastogenic for all operating room crew [6, 8, 11–13]. Accordingly, the use of automatic smoke evacuation systems that work simultaneously with the energy device seems logical. Such devices, however, are not commonly used in daily practice, mainly because of the need for another device setup, additional cost, and particularly lack of objective validation.
In this study, we used IES2 as a representative commercially available smoke evacuator. The 30-s activation of energy devices was adopted, because the visualization obtained after the 30-s activation was very similar to that in daily practice, when we surgeons rebuffed our effort to arrest hemorrhage. Although smoke was generated in the experimental setting, the field of view in the evacuator group was better than that of the control group in subjective evaluation by ten independent well-trained surgeons. Next, we sampled the surgical smoke under various conditions for quantitative analysis. The smoke tester is an authorized device for the assessment of workplace environment by semiquantifying floating carbon compounds in the air. The industrial method was used based on the reported presence of carbon compounds in surgical smokes [6, 8, 11–13]. Before semiquantifying the surgical smoke generated during abdominal surgery, we analyzed the stain components on the filter paper and compared the results with those of the absorptive membrane using a mass spectrometer. The stains on the filter paper contained various harmful chemical compounds, such as acetaldehyde, dimethylformamide, and furfural, which are all known to contain carbon, and the results were in agreement with those of the absorptive membrane. With regard to the objective evaluation of residual smoke, in HF-ESU challenge, we semiquantified the residual smoke in the abdominal cavity by using the industrial smoke-analysis device. The lesser staining the evacuator group indicated the effectiveness of instantaneous smoke evacuation during ablation, which also enhanced laparoscopic visualization. In contrast, the high stain concentration in the control group reflected a sizeable volume of surgical smoke that spread into the operating room. These data may motivate laparoscopic surgeons to retrofit the operating rooms with smoke evacuators. On the other hand, we could not demonstrate any difference in the stains in LCS challenge, when LCS showed a “clean” tissue pad. This finding indicates negligible mist production when LCS was activated without burnt sludge on the pad. The stains, however, were significantly less in the evacuator group when sludge in the crotch was evident in the LCS. This change was due to increased mist production in the presence of “dirty” tissue pads (data not shown). These results are in agreement with our subjective findings in daily laparoscopic practice: further deterioration of visualization after repeated use of LCS without cleaning the tip. These results indicate that the use of automatic smoke evacuator also would be effective in cases with heavy use of LCS, e.g., extensive laparoscopic lymph node dissection. Stains on the membranes of retrofitted closed circuits (Fig. 3C, left side) reflect the amount of harmful substances spread into operating rooms not fitted with smoke evacuators.
We agree that this study has some limitations as follows. First, this study was performed in experimental animal settings. Chemical compounds generated by activation of energy devices in our setting would have some differences from those obtained at daily practice. Second, although the smoke tester was established device in industry, there is no evidence that the tester could be adapted for evaluation of surgical smokes. Third, the IES2 is a small sample of commercially available smoke evacuators, and we have not tested other evacuators. However, in HF-ESU challenge, the fact that subjective and objective evaluations of visualization were well correlated allows us to perform further experiments. Laparoscopic surgery is performed in the abdominal cavity isolated from room air. This indicates that it is important to filter the smoke-related harmful substances for both the patients and operating room personnel using automatic smoke evacuators. There is no doubt that the smoke evacuators available in the market need further refinement especially with regard to the activation mechanisms. For example, the IES2 only interlocks with the VIO300D electrically. Ideally, smoke evacuation should be triggered automatically by sensors that detect the surgical smoke. To help the biomedical industry manufacture such devices, we need to know the components of surgical smoke and new electrochemical sensors. In addition, the algorithm of the IES2 after activation has a space to improvement. As shown in Fig. 2B and Movie 1, visualization of surgical fields have no difference in 10 s after activation of a HF-ESU suggests that smoke evacuators should be in maximum output more rapidly. These data should be feedback to medical equipment manufacturers to develop the ideal evacuator.
Conclusions
The results of the present study demonstrated that the use of automatic smoke evacuators enhanced the field-of-view and reduced exposure to harmful compounds and the surgical smoke generated during electrosurgery in experimental laparoscopic surgery. Further studies are necessary to validate the effectiveness of such devices in the clinical settings.
References
Mattes D, Silajdzic E, Mayer M, Horn M, Scheidbach D, Wackernagel W, Langmann G, Wedrich A (2010) Surgical smoke management for minimally invasive (micro) endoscopy: an experimental study. Surg Endosc 24:2492–2501
Thiebaud H, Knize M, Kuzmicky P, Hsieh D, Felton J (1995) Airborne mutagens produced by frying beef, pork and a soy-based food. Food Chem Toxicol 33:821–828
Al Sahaf O, Vega-Carrascal I, Cunningham F, McGrath J, Bloomfield J (2007) Chemical composition of smoke produced by high-frequency electrosurgery. Ir J Med Sci 176:229–232
Barrett W, Garber S (2003) Surgical smoke: a review of the literature. Surg Endosc 17:979–987
Ott D (1998) Carboxyhemoglobinemia due to peritoneal smoke absorption from laser tissue combustion at laparoscopy. J Clin Laser Med Surg 16:309–315
Krones C, Conze J, Hoelzl F, Stumpf M, Klinge U, Moeller M, Dott W, Schumpelick V, Hollernder J (2007) Chemical composition of surgical smoke produced by electrocautery, harmonic scalpel and argon beaming-a short study. Eur Surg 39:118–121
Tomita Y, Mihashi S, Nagata K, Ueda S, Fujiki M, Hirano M, Hirahata T (1981) Mutagenicity of smoke condensates induced by CO2-laser irradiation and electrocauterization. Mutat Res 89:145–149
DesCoteaux J, Picard P, Poulin E, Baril M (1996) Preliminary study of electrocautery smoke particles produced in vitro and during laparoscopic procedures. Surg Endosc 10:152–158
Bigony L (2007) Risks associated with exposure to surgical smoke plume: a review of the literature. AORN J 86:1013–1024
Ott D (1993) Smoke production and smoke reduction in endoscopic surgery: preliminary report. Endosc Surg Allied Technol 1:230–232
Sagar P, Meagher A, Sobczak S, Wolff B (1996) Chemical composition and potential hazards of electrocautery smoke. Br J Surg 83:1792
Kokosa J, Eugene J (1989) Chemical composition of laser-tissue interaction smoke plume. J Laser Appl 1:59–63
Hensman C, Baty D, Willis R, Cuschieri A (1998) Chemical composition of smoke produced by high-frequency electrosurgery in a closed gaseous environment. Surg Endosc 12:1017–1019
Acknowledgments
The authors acknowledge AMCO Incorporated, Tokyo, Japan and Simadzu Incorporated, Kyoto, Japan for their technical supports.
Disclosures
Drs. Takahashi, Yamasaki, Hirota, Miyazaki, Moon, Souma, Mori, Doki, and Nakajima report no conflict of interest or financial ties with any of the firms mentioned in this report.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Movie 1 Representative laparoscopic field of view in the two groups (left: group E; evacuator group, right: group N; control group). (MPG 3592 kb)
Movie 2 The industrial use smoke tester equipped with filter paper was connected to the working port. The residual surgical smoke stained the filter paper after ten pulls of the cylinder. (MPG 4490 kb)
Rights and permissions
About this article
Cite this article
Takahashi, H., Yamasaki, M., Hirota, M. et al. Automatic smoke evacuation in laparoscopic surgery: a simplified method for objective evaluation. Surg Endosc 27, 2980–2987 (2013). https://doi.org/10.1007/s00464-013-2821-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2821-y