Abstract
Purpose
Peptide receptor radionuclide therapy (PRRT) with 90Y and 177Lu provides objective responses in neuroendocrine tumours, and is well tolerated with moderate toxicity. We aimed to identify clinical parameters predictive of long-term renal and haematological toxicity (myelodysplastic syndrome and acute leukaemia).
Methods
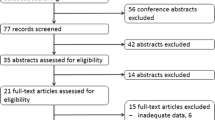
Of 807 patients studied at IEO-Milan (1997–2013), 793 (98 %) received 177Lu (278, 34.4 %), 90Y (358, 44.4 %) or 177Lu and 90Y combined (157. 19.5 %), and 14 (2 %) received combinations of PRRT and other agents. Follow-up was 30 months (1–180 months). The parameters evaluated included renal risk factors, bone marrow toxicity and PRRT features. Data analysis included multiple regression, random forest feature selection, and recursive partitioning and regression trees.
Results
Treatment with 90Y and 90Y + 177Lu was more likely to result in nephrotoxicity than treatment with 177Lu alone (33.6 %, 25.5 % and 13.4 % of patients, respectively; p < 0.0001). Nephrotoxicity (any grade), transient and persistent, occurred in 279 patients (34.6 %) and was severe (grade 3 + 4) in 12 (1.5 %). In only 20–27 % of any nephrotoxicity was the disease modelled by risk factors and codependent associations (p < 0.0001). Hypertension and haemoglobin toxicity were the most relevant factors. Persistent toxicity occurred in 197 patients (24.3 %). In only 22–34 % of affected patients was the disease modelled by the clinical data (p < 0.0001). Hypertension (regression coefficient 0.14, p < 0.0001) and haemoglobin toxicity (regression coefficient 0.21, p < 0.0001) were pertinent factors. Persistent toxicity was associated with shorter PRRT duration from the first to the last cycle (mean 387 vs. 658 days, p < 0.004). Myelodysplastic syndrome occurred in 2.35 % of patients (modelled by the clinical data in 30 %, p < 0.0001). Platelet toxicity grade (2.05 ± 1.2 vs. 0.58 ± 0.8, p < 0.0001) and longer PRRT duration (22.6 ± 24 vs. 15.5 ± 9 months, p = 0.01) were relevant. Acute leukaemia occurred in 1.1 % of patients (modelled by the clinical data in 18 %, p < 0.0001).
Conclusion
Identified risk factors provide a limited (<30 %) risk estimate even with target tissue dosimetry. These data strongly suggest the existence of unidentified individual susceptibilities to radiation-associated disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peptide receptor radionuclide therapy (PRRT) has been administered for almost two decades and is an established effective therapeutic approach in the treatment of inoperable or metastatic gastroenteropancreatic (GEP), bronchopulmonary and other neuroendocrine tumours (NETs). The two most commonly used radiopeptides, 90Y-octreotide and 177Lu-octreotate, produce objective response rates of 15–35 % [1–6]. However, no randomized trials have been performed, and the results of an ongoing phase III study are projected for 2016 (http://netter-1.com/). In addition to tumour shrinkage, biochemical and symptomatic responses are commonly observed [7]. Of particular relevance is the favourable outcome in terms of both progression-free survival and overall survival [8, 9].
In general, PRRT is well tolerated with moderate toxicity in the majority of patients if the necessary precautions (e.g. coadministration of amino acids) are undertaken [1, 9]. Nevertheless, long-term adverse events remain poorly understood and are often unpredictable, and rigorous data relating to this substantial clinical issue are limited [10]. The critical targets of long-term toxicity are the kidneys and bone marrow, with loss of renal function (grade 3/4 toxicity in 3–9 % of patients after treatment with 90Y peptide, grade 4 toxicity 0.4 % after treatment with 177Lu peptide), reduced bone marrow reserve and, more infrequently, myelodysplastic syndrome (MDS) and leukaemias (sporadically reported) [1, 2, 4, 9, 10]. Haematological toxicity is the most common subacute side effect of bone marrow irradiation. The nadir usually occurs 4–6 weeks after therapy, and toxicity is mild and reverses within a few weeks of treatment cessation. More severe WHO grade 3 or 4 haematological toxicities occur in about <10 % of patients irrespective of the radiopeptide [1, 10].
Renal irradiation occurs as a consequence of proximal tubular reabsorption of filtered radiopeptides with radiation to the glomeruli [2, 11, 12]. In such circumstances, the development of thrombotic microangiopathy may culminate in permanent renal toxicity 6–12 months after irradiation [11, 12]. Irrespective of protection, PRRT leads to a reduction in kidney function with a loss of creatinine clearance of 4 % and 7 % per year for 177Lu-octreotate and 90Y-octreotide, respectively [9]. It has been reported that a higher and more persistent decline in creatinine clearance is more frequent when renal risk factors such as longstanding or poorly controlled diabetes, previous platinum-based chemotherapy and hypertension are present [13, 14].
Therapy-related myeloid neoplasms, MDS and acute leukaemia (AL), are part of a spectrum of single disease entities whose pathobiology remain unknown and which may be a lethal late complications of cytotoxic treatment for a primary cancer [15]. The precise causal relationship with PRRT remains elusive since only a small percentage of patients (about 2 % after 177Lu-octreotate therapy) develop the syndrome [4, 8, 10]. An association with collateral myelotoxic therapy including chemotherapy or radiotherapy has, however, been suggested [2, 10]. Radioiodine, with physical characteristics similar to Lutetium, can induce second primary tumors with a probability comparable to external radiotherapy and lower than chemotherapy [16].
Given the increased use of PRRT in NETs and the numerous other coadministered therapies, it is crucial to define the risk relationship between toxicity and therapy by identifying risk factors. These factors are considered to modulate the occurrence of adverse events after PRRT through altering the thresholds for toxicity to critical organs [10, 13, 14]. In this study we analysed the long-term outcome of kidney and bone marrow parameters in a large cohort of patients with metastatic and/or inoperable NETs who underwent PRRT, with the intention of assessing the predictive value of clinical risk factors. Specifically, we assessed the occurrence of renal and bone marrow toxicity of any grade, evaluated the presence and strength of the correlation between toxicity and risk factors [9, 17], and evaluated the correlation between toxicity and the PRRT parameters, as well as other associated clinical features.
Materials and methods
Between February 1996 and April 2013 887 individuals with GEP, bronchial or unknown site NETs were treated with PRRT protocols at the European Institute of Oncology (IEO) in Milan. Of these, 70 with no follow-up data after the first cycle were excluded. The retrospective analysis therefore included 807 patients. Treatment protocols are shown in Table 1. Of the 807 patients, 793 (98 %) were treated with 177Lu, 90Y or the two combined and 14 (2 %) with combinations of PRRT and other agents, and 93 (11.5 %) received an adjunctive salvage PRRT treatment. The median total cumulative activity from treatment with 90Y-octreotide alone was 10.1 GBq (range 1.1–26.5 GBq), from 177Lu-octreotate alone was 23.3 GBq (1.7–49.2 GBq) and from the combination treatment was 7.3 GBq from 90Y and 13.44 GBq from 177Lu (ranges 0.4–31.7 and 1.1–39 GBq, respectively). Patients received various treatment schemes, which were mainly selected on the basis of response and frequently adapted to the clinical scenario (e.g. toxicity). In some instances treatment was stopped early due to significant disease progression. Nevertheless, these individuals are included in the analysis.
Analysis of parameters
The following parameters were included in the analysis: age at diagnosis, gender, tumour site, tumour grade, Ki67 (highest value), FDG positivity, clinical syndrome, metastases and site (liver, lymph nodes, bone, lung, peritoneum, other), therapy with somatostatin analogues, and previous therapy, including surgical resection of the primary, chemotherapy, radiotherapy, interferon, transarterial (chemo)embolization (TACE, TAE) and radiofrequency ablation. The following risk factors for nephrotoxicity were also included: diabetes (controlled/uncontrolled), hypertension (controlled/uncontrolled), and other factors, such as chemotherapy with nephrotoxic agents, TACE or TAE, renal NET lesions, kidney encasement by a tumour lesion, renal tumours or cysts, congenital or acquired absence of one kidney, congenital or acquired kidney malformation, nephrolithiasis, renal outflow obstruction, reduced renal function at baseline and kidney diseases (autoimmune, acquired). The following bone marrow risk factors were included: chemotherapy with myelotoxic agents and other factors, such as tumour invasion of bone marrow, radiotherapy (bone marrow fields), immunosuppressive agents, previous radionuclide therapies with 131I or 131I-MIBG, previous bone marrow toxicity, previous anaemia (including minor/minimal beta-thalassaemia, macrocytosis, leucopenia, thrombocytopenia and monoclonal gammopathies), and prior myeloproliferative diseases including myelogenous leukaemia in one patient and lymphoblastic leukaemia in one.
Toxicity parameters included haematological toxicity grade (worst grade during follow-up) evaluated as haemoglobin (Hb), white blood cell (WBC) count and platelet (PLT) count, whether haematological toxicity grade 2 or more persisted after PRRT, creatinine toxicity grade, whether renal toxicity grade 1 or more persisted after PRRT, creatinine clearance with persistent toxicity of any grade, MDS and AL. These were also tested separately as codependent associations with toxicity, together with the cumulative administered activity (in microcuries), number of cycles, approximate activity per cycle, and the type of radiopeptide used.
Other clinical factors considered in the analysis were the date of diagnosis, the date of the start and end of PRRT, salvage/adjunctive PRRT, and the date of the start and end of salvage/adjunctive PRRT. Cohort parameters included: last follow-up or contact, length of follow-up, whether the individual was alive, date of death, and if death was NET-related, as determined from the institutional tumour registry. Clinical information was obtained from hospital charts (including inpatient episodes and outpatient visits), when feasible, and when unavailable, from patient contact (phone calls, faxes, emails). Haematological criteria were assessed biweekly during PRRT treatment, monthly in the first year of follow-up, and every 3–6 months in the subsequent period, until death, loss to follow-up, or a different treatment was initiated. In a subset of 34 patients, dosimetric data were available and could be correlated with outcome (Table 2). According to previously published data, a lower renal threshold for toxicity (biologically effective dose, BED, 30 Gy) was considered in patients with risk factors, in contrast to 40 Gy in those without such factors [13, 14]. The conventional threshold of 2 Gy was considered for the bone marrow.
Toxicity parameters
Toxicity was graded according to Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 (NCI, Bethesda, MD.).
Statistical analysis
Multiple regression and data subanalysis
Multiple linear regression analysis was undertaken. The variables to model the disease (e.g., nephrotoxicity) in the dataset of 807 patients included known clinical risk factors (six covariates, e.g. previous chemotherapy) and codependent associated factors (eight covariates, e.g. Hb toxicity). Four outcomes were modelled: (1) any nephrotoxicity (any grade, including transient; 279 patients); (2) persistent not recovering nephrotoxicity (197 patients); (3) MDS (19 patients); and (4) AL (8 patients). Nephrotoxicity was defined as any transient or persistent elevation in creatinine (nonrenal causes of creatinine elevation were excluded a priori). Covariates were binary coded: no 0, yes 1. For subanalyses, age and Hb toxicity grade were analysed as a continuous variable while other variables (e.g. gender) were evaluated as discrete variables using the chi-squared test. The Mann-Whitney U test (nonparametric, two-tailed) was also used when applicable (SPSS version 22, GraphPad Software Prism 6.0).
Analysis of the importance of clinical features
The importance of individual clinical features for predicting nephrotoxicity and MDS was calculated using random forest and bootstrap aggregation for an ensemble of 1,000 decision trees (R package randomForest, R version 3.0.1). The mean decrease in Gini coefficient was used as a measure of the importance of a variable. Variable importance ≥10 and ≥1 was used to select features for prediction of nephrotoxicity and MDS, respectively.
Recursive partitioning and regression analysis
Regression trees predicting the development of nephrotoxicity and MDS were constructed from 38 variables using the rpart package [18] for the R computational environment (R version 3.0.1). The development of nephrotoxicity and MDS were analysed as discrete variables.
Results
Dataset audit
The study included 807 patients. Demographics included male gender (57.2 %) and average age at diagnosis (53.1 years, range 9.54–85 years). Tumour sites included carcinoid of unknown primary (CUP; 93 patients, 11.5 %), gut (276 patients, 34.2 %), pancreas (329 patients, 40.8 %) and bronchopulmonary NETs (109 patients, 13.5 %). In order to assess all observed toxicities, three treatment groups were considered based on the radiopeptide used: 177Lu alone (290 patients, 35.9 %), 177Lu and 90Y (157 patients, 19.5 %) and 90Y alone (360 patients, 44.6 %). The mean number of treatment cycles was 4.75 (range 1–19) in particular, 5.1 for lutetium, 5.6 for yttrium + lutetium, and 4.4 for yttrium. The average duration of PPRT, including salvage treatments, was 14.6 months (range 0–108.1 months). The median duration of follow-up was 30 months (range 1–180 months).
Renal toxicity, defined as an increase of any grade in serum creatinine, transient or persistent, in the entire group of 807 patients, occurred in 279 patients (34.6 %). Renal toxicity was temporary and mild (grade 1/2) in 29.4 % of them. Persistent toxicity occurred in 197 patients (70.6 %), and in the majority these 197 patients (93.9 %) toxicity was mild, but severe (grade 3/4) toxicity was noted in 6.1 % of these 197 (1.5 % of the whole group of 807 patients; Table 3). The corresponding percentage loss in creatinine clearance (Cockroft-Gault formula) could be retrieved in 162 of the 197 patients with persistent toxicity (Table 4).
Haematological toxicity (PLT, WBC or Hb) was mild or absent in the large majority of patients. Grade 1/2 toxicity occurred in 663 patients (82.2 %). Severe (grade 3/4) toxicity occurred in 9.5 % of patients (Table 5).
Comparison of 90Y-based and 177Lu-based therapies
Prior to the inclusive analysis (807 patients), we determined whether there were differences among the patients of the three treatment groups. Before 1999, when amino acid-based renal protection was introduced, 42 patients (5.2 %) were treated with 90Y. This group exhibited significantly higher rates of nephrotoxicity (any form in 25, 60 %; persistent in 19, 45 %), than the post-1999 cohort (any form in 254, 33.2 %; persistent in 177, 23.1 %; χ 2 = 9.4 and 11.1, p < 0.002). No significant differences were noted for the development of MDS (2.4 % vs. 2.5 %) or AL (0 % vs. 1.05 %).
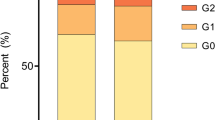
90Y treatment overall (before and after 1999) was associated with significantly higher rates of any nephrotoxicity (43.9 %) and persistent toxicity (33.6 %) than 177Lu treatment (25.5 % and 13.4 %, p < 0.0001; Fig. 1a). Overall, nephrotoxicity of any grade occurred in 279 patients (34.6 %) but was severe only in 1.5 % (Fig. 1b). Combination therapy (90Y + 177Lu) also resulted in a higher proportion of persistent nephrotoxicity (23.6 %, p < 0.0001) than 177Lu treatment alone. No differences were noted in gender distribution but the use of somatostatin analogues was higher in the 177Lu-treated group (269 patients, 92.8 %) than in the 90Y-treated group (271 patients, 75.3 %; p < 0.0001).
Comparison of the three treatment groups, 177Lu (290 patients), 177Lu/90Y combination (157 patients) and 90Y alone (360 patients. a Development of nephrotoxicity. MDS and AL in the three treatment groups. 90Y + 177Lu and 90Y alone were associated with significantly higher levels of nephrotoxicity. The data are presented as means (*p < 0.0001 vs. 177Lu alone, two-tailed Mann-Whitney U test). LU 177Lu, LU + YT combination, YT = 90Y. b Nephrotoxicity, transient and persistent (grade 1/2), occurred in 279 patients (34.6 %) and was severe (grade 3/4) in 1.5 %
Analysis of potential clinical factors associated with the development of nephrotoxicity or MDS/AL identified significant differences for previous chemotherapy and radiotherapy as well as for other nephrotoxic risk factors. Specifically, a significantly lower (both p < 0.03) percentage of the 177Lu group was exposed to previous chemotherapy (83 patients, 28.6 %) and radiotherapy (9 patients, 3.1 %) than of the 90Y group (134 patients, 37.2 %; 27 patients, 7.5 %, respectively). Neither uncontrolled diabetes nor hypertension were different between the groups, but the 90Y group exhibited a higher percentage of other nephrotoxic risk factors (140 patients, 38.9 %, vs. 90 patients, 31 %; p < 0.05).
Inclusive comparative analysis
To investigate the study hypothesis, the entire group of 807 patients was included.
Any nephrotoxicity
This analysis included 279 patients (34.6 %) with any nephrotoxicity including transient. In 20 % of affected patients the disease was modelled by the risk factor data (adjusted R 2 = 0.032, F = 5.46, p < 0.0001). Codependent associations modelled the disease in 27 % of affected patients (adjusted R 2 = 0.063, F = 7.78, p < 0.001). Variables significantly related to the development of nephrotoxicity are shown in Table 6. Of the known risk factors, hypertension and other risks for nephrotoxicity, e.g. nephrotoxic chemotherapy and TACE, were significantly associated with the development of nephrotoxicity. Of the codependent associative factors, Hb toxicity grade was most significantly related to the development of disease, possibly as a consequence of nephrotoxicity. Other factors included the number of cycles. However, the combination of 177Lu and 90Y was negatively associated, i.e. inversely related to the development of nephrotoxicity. Subanalysis showed that Hb toxicity grade was higher in patients with nephrotoxicity (1.30 ± 0.74 vs. 1.0 ± 0.73, p < 0.0001; Fig. 2a), and these patients were older (56.7 ± 12.3 years vs. 52.6 ± 13.2 years, p < 0.0001; Fig. 2b) and were more frequently men (63.4 % vs. 53.9 %, p < 0.05; Fig. 2c), and nephrotoxicity occurred more often in those receiving 90Y or a combination of 177Lu and 90Y (73.5 % vs. 59 %, p < 0.05; Fig. 2d).
Risk factors and codependent clinical features associated with development of nephrotoxicity following PRRT treatment. A higher Hb grade (a) and older age (b) as well as male gender (c) were all positively linked. 177Lu treatment was negatively related to the development of disease (d). The creatinine grade was not related to PRRT exposure (e) but patients who developed nephrotoxicity had a significantly lower time of exposure to radiation (f). The data are presented as means ± SEM (*p < 0.0001 vs. no nephrotoxicity, # p < 0.01 vs. transient nephrotoxicity; two-tailed Mann-Whitney U test). No No nephrotoxicity, Yes development of any nephrotoxicity, M male, F female, Other 177Lu + 90Y treatment and 90Y treatment, PERS persistent nephrotoxicity, TRANS transient nephrotoxicity
Persistent nephrotoxicity
This analysis included 197 patients (24.3 %) with persistent nephrotoxicity. Clinical risk factors modelled the disease in 22 % of affected patients (adjusted R 2 = 0.038, F = 5.82, p < 0.0001). Codependent associations modelled the disease in 34 % of affected patients (adjusted R 2 = 0.104, F = 11.5, p < 0.001). Variables significantly related to persistent nephrotoxicity are shown in Table 6. The variables associated with persistent nephrotoxicity were the same as those for any grade of nephrotoxicity except that other previous therapies were included in the model. Codependent associations included Hb toxicity and the number of cycles as positively related to persistent nephrotoxicity, while the radiopeptide type (177Lu and 177Lu + 90Y, as well as the cumulative number of cycles and WBC toxicity were negatively associated with the development of persistent nephrotoxicity.
Subanalysis showed that Hb toxicity grade was higher in patients with persistent nephrotoxicity (1.42 ± 0.75 vs. 1.024 ± 0.62, p < 0.0001) and more patients were exposed to 90Y-based PRRT (83 % vs. 59 %, p < 0.05). There was no relationship between the grade of nephrotoxicity and the duration of PRRT exposure from the first to the last cycle (Fig. 2e). However, individuals who developed persistent toxicity had a significantly shorter duration of PRRT exposure (mean 387 days vs. 658 days for transient toxicity, p < 0.004; Fig. 2f). Subanalysis of transient versus persistent nephrotoxicity did not identify any known clinical risk factor; Hb toxicity grade was the only covariate identified as significantly different (1.42 ± 0.75 vs. 1.02 ± 0.63, p < 0.0001).
MDS
MDS occurred in 19 patients (2.35 %). Clinical risk factors modelled the disease in 16 % of affected patients (adjusted R 2 = 0.02, F = 5.16, p < 0.0001) whereas codependent associations modelled the disease in 30 % of affected patients (adjusted R 2 = 0.08, F = 9.9, p < 0.0001). The risk factors associated with MDS were previous chemotherapy and other bone marrow risk factors, such as tumour invasion of bone marrow and other previous myelotoxic therapies, while the PLT toxicity grade was also significant (p = 0.01; Table 7).
Acute leukaemias
AL occurred in eight patients (1.1 %, six of whom converted from MDS: one promyelocytic, three myeloid, three lymphoblastic and one non-specified form). In 14 % of affected patients the disease was modelled by the clinical risk factor data (adjusted R 2 = 0.015, F = 4.16, p = 0.002). Codependent associations modelled the disease in only 18 % of affected patients (adjusted R 2 = 0.021, F = 3.19, p = 0.001). As found for MDS, the only risk factors associated with AL were previous chemotherapy and other bone marrow risk factors, while PLT toxicity grade was also significant (p = 0.03; Table 7). As expected, AL and MDS were correlated. Subanalysis comparing patients with MDS who developed AL and those who did not failed to identify significant differences between the two groups. The times between the start of PRRT and the development of MDS and AL (mean 1,351 days and 1,699 days, respectively) were not significantly different. However, both conditions developed significantly later than persistent nephrotoxicity (p < 0.01; Fig. 3d).
Clinical variables associated with the development of MDS and AL following PRRT treatment. A higher PLT grade (a) and longer duration of treatment (b) were both positively linked. The receiver operating characteristic curve (c) indicated that PLT grade may have utility as a marker of MDS (AUC 0.84, p < 0.0001). Development of either MDS or AL occurred at a significantly later time point than persistent nephrotoxicity (d). The data are presented as means ± SEM (*p < 0.0001 vs. no MDS and NTOX, # p < 0.01 vs. no MDS and NTOX; two-tailed Mann-Whitney U test) No No MDS, NTOX nephrotoxicity
Relationship with the absorbed dose
Dosimetric results and a median follow-up of 60 months (range 14–181 months) were available in 34 patients (4 %; Table 2). A comparison of the clinical risk factors and codependent associated factors for kidney and bone marrow toxicity identified similar variables associated with disease, e.g. other nephrotoxicity risk factors and other bone marrow risk factors, between this group and the 807 patients. Of the 34 patients, 15 had renal doses/BED above the threshold, and 8 of these developed permanent toxicity, while among the 19 patients with doses/BED below the threshold, 3 developed permanent toxicity (Fig. 4a). With regard to the bone marrow, 3 of 29 patients with doses below the threshold exhibited myeloproliferative events, while 1 patient with a dose above the threshold had no adverse events (Fig. 4b). The kidney BED, included as a codependent associative factor in the modelling analyses, demonstrated a similar relationship to nephrotoxicity as the Hb toxicity grade (standardized coefficients of 0.144 and 0.135, respectively). The bone marrow dose did not significantly contribute to the bone marrow disease modelling.
Relationships among risk factors (red background), cumulative kidney BED (blue points) and permanent renal toxicity (red circle) in the 34 patients with dosimetric estimates (a). Unless very high doses to the kidneys are administered, there is a grey zone of unpredictable outcome around the threshold (red and green circles thresholds for risk factors and absence of risk factors, respectively), in which neither the presence of risk factors nor exceeding the threshold is invariably associated with toxicity. However, risk factors were confirmed to be a discriminant, as they are more frequently associated with toxicity. b There is no correlation between the cumulative absorbed dose to the bone marrow and the occurrence of myeloproliferative events (dotted line 2-Gy threshold considered for bone marrow toxicity)
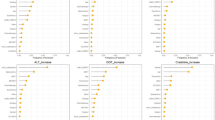
Recursive partitioning and regression tree analysis
To determine whether clinical information alone could be used to determine the risk of pathology, a classification tree analysis was constructed. The variables relating to nephrotoxicity (based on the creatinine grade) were evaluated (Fig. 5a, b) and MDS (Fig. 5c, d).
Overall, age at diagnosis, time between diagnosis and PRRT, cumulative activity, duration of PRRT, and 90Y and 177Lu doses were important determinants of nephrotoxicity (Fig. 5a). The decision tree analysis demonstrated that nephrotoxicity was not manifested in the majority of patients receiving 177Lu at commonly used cumulative doses of >200 mCi (7.4 GBq, 76 % of patients; Fig. 5b). Interestingly, development of nephrotoxicity in patients receiving <7 GBq of 177Lu required computational evaluation of additional parameters including number of cycles (>1.5), time between diagnosis and the start of PRRT (‘Time.bw.’), age (≥50 years), and 90Y activity (Fig. 5b). For example, if ‘Time.bw.’ was <31 months, the following variables were associated with the development of nephrotoxicity: age (≥50 years), WBC toxicity (≥1.5), and the use of 90Y. Sixty-four per cent (64 %) Of the patients treated with PRRT later than 31 months after diagnosis developed nephrotoxicity, as did 64 % of those treated with 90Y.
Figure 5c highlights the relative importance of each variable in the development of MDS. The analysis showed that AL, cumulative activity, duration of PRRT, age at diagnosis, time between diagnosis and PRRT, toxicity grades (PLT, WBC and Hb) and number of cycles were all important. The decision tree analysis, however, only showed that AL was a determinant of MDS (Fig. 5d). Due to the limited availability of dosimetric estimates in the entire cohort (4 %), these parameters could not be included in the analysis.
Discussion
In this retrospective analysis, we identified several risk factors and associated variables related to the development of renal and bone marrow toxicity. Of relevance was the demonstration using mathematical modelling analyses that known risk factors had limited predictive value (<25 %) for adverse events. Of interest was the identification that codependent clinical factors, e.g. Hb toxicity, were more informative than risk factors in our modelling analyses. Of further importance was the observation that analysis of the subgroup with dosimetry confirmed previous assessments of the inability of individual dosimetric estimates to accurately predict the effect at the target tissue, particularly when not significantly higher than the threshold [19]. This was most evident for bone marrow disease. These data suggest that substantial information remains unknown regarding the intrinsic biological sensitivities in individual patients. It is likely that a refined genetic and microdosimetric delineation of renal tubular and microvascular cell compartments as well as of marrow cell precursor analysis will be needed to elucidate such mechanisms and assess sensitivity to PRRT.
We evaluated 807 individuals treated with PRRT in a single centre, regardless of the completion of treatments or the response to them, in order to capture all possible clinical variables and limit any selection bias in the data analyses. Our data confirm that PRRT is a relatively safe therapeutic procedure, with a low occurrence of severe toxicity. We also confirmed that PRRT with 177Lu-octreotate was safer than with 90Y-octreotide, alone or in combination, both in terms of haematological/renal toxicity and outcomes [1, 9, 13, 17, 20].
Nephrotoxicity analysis
90Y-octreotide was confirmed to be associated with significantly higher nephrotoxicity, particularly in patients treated before the advent of renal protection with amino acids in 1999. Combination therapy also resulted in a higher proportion of patients with persistent nephrotoxicity than 177Lu alone. This may be related to the physical characteristics of the two radioisotopes. Because of its the higher energy and longer penetration range, 90Y irradiates the renal interstitium glomeruli more extensively than 177Lu. The nature of long-term kidney damage, in fact, reflects the failure to regenerate functional tissue after the initial apoptotic phenomena triggered by the irradiation, and is sustained by radiation-induced late damage to the vasculature, typically involving the glomeruli, arterioles and small arteries, and by associated tubular atrophy and interstitial fibrosis [21].
Among the risk factors the clinical feature most significantly associated with toxicity was hypertension followed by other nephrotoxic risk factors. This confirms that renal toxicity is more likely, as well as more marked, in individuals with hypertension, lesions involving the kidneys, etc. These are considered as the main risk factors for renal function impairment [9, 17]. Despite these associations, it was not possible to differentiate transient from persistent nephrotoxicity, which suggests that other factors are involved in development of higher grade kidney insufficiency. When analysing the codependent clinical variables, Hb toxicity grade was the only significant associated factor. This factor was also the only measure that could differentiate between transient and persistent nephrotoxicity. Anaemia is a consequence of reduced renal function, due to the reduced production of erythropoietin, and is also a consequence of chronic illness. Reports indicate that renal toxicity is associated with a higher frequency of haematological toxicity [9, 14].
Of interest, a subanalysis also identified that older age, male gender and the use of 90Y or combinations of 90Y were associated with a significantly higher incidence of these events. The higher incidence in males was surprising, but could reflect the greater muscular mass in men. Possible, oestrogen-modulated, lower sensitivity to free radical injury in females has also been postulated [22]. Based on this information, it would seem prudent when considering PRRT to adapt the regimen (particularly if 90Y is selected) or switch to 177Lu in individuals with long-standing hypertension. In addition, the associated clinical variables, e.g. Hb toxicity, should be used to reevaluate the regimen during the treatment protocol.
Of considerable significance in the nephrotoxicity group was the observation that modelling using multiregression analysis of risk factors and clinical data was predictive in less than 30 % of patients. Moreover, no association was noted between nephrotoxicity grade and duration of PRRT exposure. In contrast, those who developed persistent nephrotoxicity had a significantly shorter duration of radiation exposure from the first to the last cycle. To potentially explain the known limitations of dosimetry in accurately predicting toxicity in all cases, clinical factors were considered as they have been demonstrated to offer a better correlation with the outcome [13]. Our findings indicate, however, that other factors (about 70 %) are involved in the development of kidney-associated radiation toxicity. The currently available dosimetry models are not suited to measure the actual radiation doses at a micro-level such as the glomeruli specifically. We postulate these other factors are intrinsic biological determinants, possibly of genetic origin, as our analysis of kidney BED data did not identify this to be any more informative than Hb toxicity grade. The sample studied with dosimetry offered some additional insight into the underlying pathobiological phenomena and supports our modelling data. Unless very high doses were delivered to the kidneys, a zone of unpredictable outcome was noted around the threshold, in which neither risk factors nor exceeding the threshold were invariably associated with toxicity. To overcome these limitations, radiobiological models that factor in individual characteristics such as radiosensitivity are currently being developed to better correlate the target tissue effect [23].
Since creatinine clearance was not available in the entire cohort, we utilized serum creatinine as a marker of renal toxicity. This reflected the relative unavailability of direct medical follow-up information (particularly long-term) leading to the utilization of indirectly acquired material via personal patient communication. Thus, some information, e.g. body weight used to calculate the creatinine clearance with the Cockroft-Gault formula, was not consistently available. Serum creatinine provides a general estimate of renal function but underestimates the underlying renal phenomena. Additionally, if muscle mass is increased as a consequence of effective therapy, it may overestimate the actual reduction in renal function and, therefore, be a confounding factor [24]. It is generally considered, however, that an increase in creatinine values after PRRT reflects a decrease in creatinine clearance, since there is a decrease in renal function following the therapy [3, 13, 14, 25]. A subanalysis of the course of creatinine clearance obtained in 162 of the 197 patients with persistent nephrotoxicity suggested a parallel increasing percentage loss as the serum creatinine toxicity grade increases.
Long-term haematological toxicity analysis
Many marrow-related events observed after PRRT occur but are usually unexpected given the low estimated bone marrow absorbed dose. In the current study, risk factors associated with bone marrow toxicity were previous chemotherapy and other bone marrow risk factors such as previous myelotoxic therapies and anaemia. When analysing the codependent clinical variables, PLT toxicity grade was the only significantly associated factor. As confirmed in our subgroup, individual dosimetry was more accurate for the kidney, due to the model used for calculation [9, 26, 27]. This suggests that a more specific model including additional parameters should be designed for bone marrow.
The incidence of MDS and AL in the cohort analysed was 2.35 % and 1.1 %, respectively. These number, while relatively small, are of considerable consequence at a clinical level and are similar to earlier reports from Rotterdam regarding the outcome of PRRT with 177Lu-octreotate [8]. However, an incidence lower than the 5 % has been reported for 131I, whose characteristics of β-emission closely resemble those of 177Lu (Dusseldorf Myelodysplastic Syndromes Register) [28]. Secondary MDS or AL following radionuclide therapies are considered a rare stochastic event, that is without a threshold but with a probability increasing with the absorbed dose [29]. The induction of secondary malignancies by radiation is a complex process that originates as a result of single or double strand breaks in the DNA and involves errors in the repair mechanisms leading to genetic mutations, with loss of function or oncogene activation. A critical parameter in this process is the different sensitivities of DNA to radiation during the various phases of the cell cycle.
Myeloid neoplasms are considered a consequence of mutational events induced by cytotoxic therapies, or to arise via the selection of a myeloid clone with a mutator phenotype that has a markedly elevated risk for mutational events [30]. The latency between primary diagnosis and therapy-related disease ranges from a few months to more than 10 years, depending on the cumulative dosage or dose-intensity of the preceding therapy as well as the exposure to specific agents [29]. In our series, the times between PRRT and the development of MDS and AL (mean 1,351 days and 1,699 days, respectively) did not occur significantly different, but both diseases developed significantly later than persistent nephrotoxicity. This reflects two different pathogenic mechanisms. In the latter, an evolving angiopathy with ischaemic consequences and in the former, radiation-induced clonal selection followed by genetically induced or regulated proliferative events in the bone marrow [31]. In our series, the variable most significantly associated with MDS was AL (usually the consequence of MDS in the forms characterized by slow development) as well as the duration of PRRT and PLT toxicity grade. The duration of PRRT from the first to the last cycle probably reflects the continuous insult to the bone marrow, with an accumulation of mutations that lead to the development of the myeloid neoplasm. PLT toxicity grade may reflect the underlying continuing bone marrow cell damage that will result in the development of a secondary malignancy. PLT toxicity may provide some utility as a marker. When a cut-off of 1 was applied, it exhibited a sensitivity and specificity of about 70 % for predicting the development of MDS. Of note however, 8.3 % of individuals with a PLT toxicity threshold of >1 did not develop MDS. Contrary to what might have been expected, previous chemotherapy was not identified as a risk factor. Despite the fact that MDS/AL occur more frequently after chemotherapy, the prevailing concept that PRRT-associated MDS/AL develops preferentially in association with extensive pretreatment with chemotherapeutic agents may require reevaluation.
In our series, the data collected with the follow-up do not allow us to differentiate the MDS in the 19 patients into the various WHO categories (refractory anaemia, refractory anaemia with excess blasts, etc.). Moreover, the AL group (eight patients) also included those with promyelocytic and lymphoblastic forms–the latter apparently not related to the exposure to myelotoxic therapies. This suggests that a mutation event entirely related to PRRT exposure, or a stochastic event or individual susceptibility to PRRT and/or other myelotoxic therapies, is worthy of consideration.
As to the causative event, in our series, neither the amount of administered radioactivity nor the type of radionuclide employed had a significant impact on the occurrence of marrow neoplasms. In the subgroup with dosimetry, the bone marrow dose was not correlated with the development of marrow neoplasia. This, together with the observation that in only 16–30 % of patients with MDS and in 14–18 % of those with AL could the disease be modelled by clinical risk factors and coassociative factor data, indicates that intrinsic, genetically determined, factors may play a role in these events. Data from the literature, relating mainly to radioiodine therapy for thyroid diseases, indicate no difference in the incidence of myeloid neoplasms between high activities for cancer and low activities for benign diseases. This would support our hypothesis of a preexisting biological susceptibility to a radiation-induced effect, at least for commonly administered activity levels [28].
Using mathematical modelling based upon decision tree-based analysis, we identified a number of decision nodes that may potentially be useful in PRRT: the level of cumulative activity, haematological toxicity, number of cycles and treatment with 90Y are important factors for the development of nephrotoxicity. The decision tree was less informative regarding MDS and AL, but cumulative activity, duration of PRRT, age at diagnosis, time between diagnosis and PRRT and haematological disturbances, especially platelet toxicity, appeared to be important factors. The action fork identified a divide for the development of nephrotoxicity at 31 months between diagnosis and PRRT. A possible interpretation is that an interval of <31 months may indicate that the patient had not deteriorated as a result of multiple treatments, and intrinsic factors such as age could play an important role. If the interval was longer, and the patient had deteriorated (possibly as a result of multiple therapies or the disease), then development of haematological toxicity to PRRT and the type of treatment, for example 90Y, played an important role.
Conclusion
In conclusion, our observations indicate that toxicity was related to exceeding the individual threshold of tolerance of the involved organs in a particular individual. Overall, the level of intolerance to PRRT could be associated with a variety of risk and coassociated clinical features. However, these clinical variables and dosimetry only enable partial modelling [27]. The inescapable conclusion is that individual susceptibility to adverse sequelae of PRRT requires rigorous delineation of mechanistic biological events, which are likely to have a specific, individual genetic basis. Until these are identified, the guiding principle in PRRT should be the minimal effective rather than the maximum tolerated activity.
References
Kwekkeboom DJ, Mueller-Brand J, Paganelli G, Anthony LB, Pauwels S, Kvols LK, et al. Overview of results of peptide receptor radionuclide therapy with 3 radiolabeled somatostatin analogs. J Nucl Med. 2005;46 Suppl 1:62s–6s.
Bodei L, Ferone D, Grana CM, Cremonesi M, Signore A, Dierckx RA, et al. Peptide receptor therapies in neuroendocrine tumors. J Endocrinol Invest. 2009;32:360–9.
Bodei L, Cremonesi M, Grana CM, Fazio N, Iodice S, Baio SM, et al. Peptide receptor radionuclide therapy with 177Lu-DOTATATE: the IEO phase I-II study. Eur J Nucl Med Mol Imaging. 2011;38:2125–35. doi:10.1007/s00259-011-1902-1.
Imhof A, Brunner P, Marincek N, Briel M, Schindler C, Rasch H, et al. Response, survival, and long-term toxicity after therapy with the radiolabeled somatostatin analogue [90Y-DOTA]-TOC in metastasized neuroendocrine cancers. J Clin Oncol. 2011;29:2416–23. doi:10.1200/jco.2010.33.7873.
Bushnell Jr DL, O’Dorisio TM, O’Dorisio MS, Menda Y, Hicks RJ, Van Cutsem E, et al. 90Y-edotreotide for metastatic carcinoid refractory to octreotide. J Clin Oncol. 2010;28:1652–9. doi:10.1200/jco.2009.22.8585.
Kwekkeboom DJ, Teunissen JJ, Bakker WH, Kooij PP, de Herder WW, Feelders RA, et al. Radiolabeled somatostatin analog [177Lu-DOTA0, Tyr3]octreotate in patients with endocrine gastroenteropancreatic tumors. J Clin Oncol. 2005;23:2754–62. doi:10.1200/jco.2005.08.066.
Khan S, Krenning EP, van Essen M, Kam BL, Teunissen JJ, Kwekkeboom DJ. Quality of life in 265 patients with gastroenteropancreatic or bronchial neuroendocrine tumors treated with [177Lu-DOTA0, Tyr3]octreotate. J Nucl Med. 2011;52:1361–8. doi:10.2967/jnumed.111.087932.
Kwekkeboom DJ, de Herder WW, Kam BL, van Eijck CH, van Essen M, Kooij PP, et al. Treatment with the radiolabeled somatostatin analog [177Lu-DOTA 0, Tyr3]octreotate: toxicity, efficacy, and survival. J Clin Oncol. 2008;26:2124–30. doi:10.1200/jco.2007.15.2553.
Kwekkeboom DJ, Kam BL, van Essen M, Teunissen JJ, van Eijck CH, Valkema R, et al. Somatostatin-receptor-based imaging and therapy of gastroenteropancreatic neuroendocrine tumors. Endocr Relat Cancer. 2010;17:R53–73. doi:10.1677/erc-09-0078.
Frilling A, Modlin IM, Kidd M, Russell C, Breitenstein S, Salem R, et al. Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol. 2014;15:e8–e21. doi:10.1016/s1470-2045(13)70362-0.
Brans B, Bodei L, Giammarile F, Linden O, Luster M, Oyen WJ, et al. Clinical radionuclide therapy dosimetry: the quest for the “Holy Gray”. Eur J Nucl Med Mol Imaging. 2007;34:772–86. doi:10.1007/s00259-006-0338-5.
Rolleman EJ, Kooij PP, de Herder WW, Valkema R, Krenning EP, de Jong M. Somatostatin receptor subtype 2-mediated uptake of radiolabelled somatostatin analogues in the human kidney. Eur J Nucl Med Mol Imaging. 2007;34:1854–60.
Bodei L, Cremonesi M, Ferrari M, Pacifici M, Grana CM, Bartolomei M, et al. Long-term evaluation of renal toxicity after peptide receptor radionuclide therapy with 90Y-DOTATOC and 177Lu-DOTATATE: the role of associated risk factors. Eur J Nucl Med Mol Imaging. 2008;35:1847–56. doi:10.1007/s00259-008-0778-1.
Valkema R, Pauwels SA, Kvols LK, Kwekkeboom DJ, Jamar F, de Jong M, et al. Long-term follow-up of renal function after peptide receptor radiation therapy with (90)Y-DOTA(0),Tyr(3)-octreotide and (177)Lu-DOTA(0), Tyr(3)-octreotate. J Nucl Med. 2005;46 Suppl 1:83s–91s.
Churpek JE, Larson RA. The evolving challenge of therapy-related myeloid neoplasms. Best Pract Res Clin Haematol. 2013;26:309–17. doi:10.1016/j.beha.2013.09.001.
Dottorini ME, Salvatori M. Is radioiodine treatment for thyroid cancer a risk factor for second primary malignancies? Clin Transl Imaging. 2013;1:205–16. doi:10.1007/s40336-013-0022-2.
Vegt E, de Jong M, Wetzels JF, Masereeuw R, Melis M, Oyen WJ, et al. Renal toxicity of radiolabeled peptides and antibody fragments: mechanisms, impact on radionuclide therapy, and strategies for prevention. J Nucl Med. 2010;51:1049–58. doi:10.2967/jnumed.110.075101.
Therneau T, Atkinson B, Ripley B. rpart: Recursive partitioning and regression times. 2014. http://cran.r-project.org/package=rpart/index.html.
Cremonesi M, Ferrari M, Di Dia A, Botta F, De Cicco C, Bodei L, et al. Recent issues on dosimetry and radiobiology for peptide receptor radionuclide therapy. Q J Nucl Med Mol Imaging. 2011;55:155–67.
Paganelli G, Sansovini M, Ambrosetti A, Severi S, Monti M, Scarpi E, et al. 177Lu-Dota-octreotate radionuclide therapy of advanced gastrointestinal neuroendocrine tumors: results from a phase II study. Eur J Nucl Med Mol Imaging. 2014. doi:10.1007/s00259-014-2735-5.
Cybulla M, Weiner SM, Otte A. End-stage renal disease after treatment with 90Y-DOTATOC. Eur J Nucl Med. 2001;28:1552–4. doi:10.1007/s002590100599.
Sabolic I, Asif AR, Budach WE, Wanke C, Bahn A, Burckhardt G. Gender differences in kidney function. Pflugers Arch. 2007;455:397–429. doi:10.1007/s00424-007-0308-1.
Strigari L, Benassi M, Chiesa C, Cremonesi M, Bodei L, D’Andrea M. Dosimetry in nuclear medicine therapy: radiobiology application and results. Q J Nucl Med Mol Imaging. 2011;55:205–21.
Lane BR, Poggio ED, Herts BR, Novick AC, Campbell SC. Renal function assessment in the era of chronic kidney disease: renewed emphasis on renal function centered patient care. J Urol. 2009;182:435–43. doi:10.1016/j.juro.2009.04.004. discussion 43–4.
Sabet A, Ezziddin K, Pape UF, Reichman K, Haslerud T, Ahmadzadehfar H, et al. Accurate assessment of long-term nephrotoxicity after peptide receptor radionuclide therapy with (177)Lu-octreotate. Eur J Nucl Med Mol Imaging. 2014;41:505–10. doi:10.1007/s00259-013-2601-x.
Cremonesi M, Botta F, Di Dia A, Ferrari M, Bodei L, De Cicco C, et al. Dosimetry for treatment with radiolabelled somatostatin analogues. A review. Q J Nucl Med Mol Imaging. 2010;54:37–51.
Walrand S, Barone R, Pauwels S, Jamar F. Experimental facts supporting a red marrow uptake due to radiometal transchelation in 90Y-DOTATOC therapy and relationship to the decrease of platelet counts. Eur J Nucl Med Mol Imaging. 2011;38:1270–80. doi:10.1007/s00259-011-1744-x.
Schroeder T, Kuendgen A, Kayser S, Kroger N, Braulke F, Platzbecker U, et al. Therapy-related myeloid neoplasms following treatment with radioiodine. Haematologica. 2012;97:206–12. doi:10.3324/haematol.2011.049114.
Godley LA, Larson RA. Therapy-related myeloid leukemia. Semin Oncol. 2008;35:418–29. doi:10.1053/j.seminoncol.2008.04.012.
Boehrer S, Ades L, Tajeddine N, Hofmann WK, Kriener S, Bug G, et al. Suppression of the DNA damage response in acute myeloid leukemia versus myelodysplastic syndrome. Oncogene. 2009;28:2205–18. doi:10.1038/onc.2009.69.
Kayser S, Dohner K, Krauter J, Kohne CH, Horst HA, Held G, et al. The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood. 2011;117:2137–45. doi:10.1182/blood-2010-08-301713.
Conflicts of interest
G.P. is consultant for AAA. D.J.K. and E.P.K. are shareholders of AAA and steering committee members of AAA's NETTER-1 study. The other authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bodei, L., Kidd, M., Paganelli, G. et al. Long-term tolerability of PRRT in 807 patients with neuroendocrine tumours: the value and limitations of clinical factors. Eur J Nucl Med Mol Imaging 42, 5–19 (2015). https://doi.org/10.1007/s00259-014-2893-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-014-2893-5