Abstract
Objective
Delirium in the critically ill is reported in 11–80% of patients. We estimated the incidence of delirium using a validated scale in a large cohort of ICU patients and determined the associated risk factors and outcomes.
Design and setting
Prospective study in a 16-bed medical-surgical intensive care unit (ICU).
Patients
820 consecutive patients admitted to ICU for more than 24 h.
Interventions
Tools used were: the Intensive Care Delirium Screening Checklist for delirium, Richmond Agitation and Sedation Scale for sedation, and Numerical Rating Scale for pain. Risk factors were evaluated with univariate and multivariate analysis, and factors influencing mortality were determined using Cox regression.
Results
Delirium occurred in 31.8% of 764 patients. Risk of delirium was independently associated with a history of hypertension (OR 1.88, 95% CI 1.3–2.6), alcoholism (2.03, 1.2–3.2), and severity of illness (1.25, 1.03–1.07 per 5-point increment in APACHE II score) but not with age or corticosteroid use. Sedatives and analgesics increased the risk of delirium when used to induce coma (OR 3.2, 95% CI 1.5–6.8), and not otherwise. Delirium was linked to longer ICU stay (11.5 ± 11.5 vs. 4.4 ± 3.9 days), longer hospital stay (18.2 ± 15.7 vs. 13.2 ± 19.4 days), higher ICU mortality (19.7% vs. 10.3%), and higher hospital mortality (26.7% vs. 21.4%).
Conclusion
Delirium is associated with a history of hypertension and alcoholism, higher APACHE II score, and with clinical effects of sedative and analgesic drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Delirium in the critically ill is common and distressing [1, 2, 3]. Although recognized since Hippocratic times [4], delirium remains difficult to diagnose and treat in the ICU [5]. Delirium incidence over 80% has been reported in critically ill patients [6, 7, 8, 9], as have threefold increases in the risk of mortality [9]. In contrast, we [10] and others [11, 12, 13, 14] have reported far lower incidence ranges (11–31%). Delirium has been termed an “organ failure” of the brain [15], analogous to other end-organ damage resulting from severe systemic disease. Common neural pathways have been invoked for coma, neurological abnormalities, and delirium [15, 16, 17, 18]. It is important to diagnose ICU delirium accurately, as treatment carries risk. Neuroleptics can be harmful [19, 20], and excess sedative use in intensive care prolongs mechanical ventilation and hospital stay [21]. We determined the incidence of delirium in a cohort of consecutive medical and surgical ICU patients using the Intensive Care Delirium Screening Checklist and evaluated associated risk factors and outcomes.
Methods
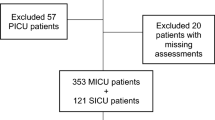
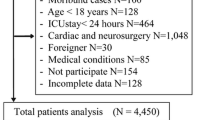
Between December 2003 and August 2004 we screened 820 consecutive patients aged 18 years or older who were admitted for more than 24 h to a medical-surgical intensive care unit (ICU) in a tertiary care university hospital (Maisonneuve-Rosemont Hospital, Montreal, Canada) Appendix [22]. Individuals unlikely to survive for 24 h were excluded. Data were collected for a total of 4,707 patient-days (mean 5.7 ± 7 days per patient). The mean Acute Physiology and Chronic Health Evaluation (APACHE) II score on admission was 16.5 ± 8.2 (range 0–59); 79% were mechanically ventilated on admission. Fifty-six patients could not be evaluated due to prolonged coma; of the remaining 764 patients 243 (31.8%) developed delirium (Fig. 1). Delirious patients had an overall score of 4/8 or more for a mean of 37.932.5% of their ICU stay. Sixty one (10.1%) remained with an elevated score at discharge. The institutional research and ethics committees approved the study protocol and waived the need for individual informed consent.
Age, gender, prior diagnoses, admission diagnosis, APACHE II score, Glasgow Coma Scale (GCS), and selected laboratory values [10] were recorded. Medical history previously associated with delirium were documented (i. e., hypertension [10], diabetes, chronic obstructive pulmonary disease, preexisting central nervous system disease including neuromuscular disorders, dementia [23], and stroke [24], renal insufficiency [25], visual or auditory impairment [26], smoking [10], alcoholism (two drinks or more daily, or weekly consumption of the equivalent of 26 oz of 40 proof alcohol) [10], and habitual drug use) [27]. The category of admission (surgical vs. medical, urgent vs. nonurgent) was noted. The medical history and data relevant to the ICU stay including laboratory values [10, 28] were obtained. Daily sedative and opiate doses, epidural analgesia use [10], and administration of two drugs associated with delirium, corticosteroids [29] and indomethacin [30], were recorded.
All patients were assessed daily and followed until death or ICU discharge. Daily and cumulative drug doses of all drugs above were recorded up to and including the day that delirium was identified, or for overall ICU stay in nondelirious patients. As a strong correlation (R2 = 0.85) was found between mean daily and cumulative doses, only daily doses are provided. All patients were evaluated by nurses every 1–8 h. Because pain has been associated with delirium [31], we employed the NRS pain assessment tool [32]. Sedation was assessed with the Richmond Agitation and Sedation Scale (RASS) [33, 34]. As patients may be sedated but anxious, all patients with RASS scores of –3 or higher were asked about anxiety, and their response recorded (i. e., “yes” or “no”). Unclear and absent responses were considered impossible to evaluate and rated “0” (i. e., the same as no anxiety).
Coma was defined as a score of 5 on the RASS scale. All comatose patients were further classified as follows: (a) medical coma (patients with conditions that fully accounted for the coma, for example, severe anoxic brain damage), (b) multifactorial coma (patients in a coma because of both medical factors and medication), or (c) induced coma (patients in whom heavy sedation accounted fully for the coma, for example, sedation for the purposes of controlled mechanical ventilation). The latter were also separated into patients who were comatose for more than 24 h (“iatrogenic coma”) and those comatose for less than 24 h following general anesthesia or sedation for procedures (“transient iatrogenic coma”). The few patients (n = 7/820, < 1%) whose ICU admission featured more than one type of coma were categorized according to the first type of coma identified. Lastly, prolonged coma was defined as coma present from the time of admission and lasting longer than 5 days or until death.
All patients were evaluated with the 8-item Intensive Care Delirium Screening Checklist (ICDSC; see Appendix I) [22] by a nurse or a physician every 1–8 h for the duration of the ICU stay. Patient with an ICDSC score of 4 or higher were considered delirious and those with a score of 3 or less were not [22]. A physician confirmed the diagnosis by clinical assessment. Coma precluding evaluation of delirium was defined as a RASS score of –5. Patients unable to undergo an assessment were noted as “not evaluated” and not labeled delirious. Follow-up to hospital discharge was completed in all patients. ICU as well as hospital length of stay and mortality were recorded.
Analysis
All patients with an ICDSC score of 4 or higher at least once were compared to those with a score of 3 or less throughout their ICU stay. APACHE scores and age independently affect mortality and length of stay in our ICU population (data not shown), and therefore both were considered. Length of stay and mortality in the ICU and after transfer to a ward were compared for “delirious” vs. “nondelirious” patients after adjusting for these confounding factors (age and APACHE II score). Since coma is a potentially confounding variable, the APACHE II score was calculated with and without the GCS component as previously described [9]. Survival was assessed by Cox regression analysis. Patients were evaluated for delirium either prior to the development of coma or when they recovered consciousness. Patients with prolonged coma could not be assessed; these cases were analyzed separately but were excluded from risk factor analysis because of their small number (n = 56). Results are reported as comparative odds ratio (OR) with 95% confidence interval (CI).
Narcotic analgesics were converted into morphine equivalents [32], benzodiazepines into lorazepam equivalents [35], and corticosteroids into prednisone equivalents [36]. Propofol and indomethacin doses were recorded directly. Univariate logistic regression was used with an α criterion of 0.15 to select variables that differentiated “delirium” vs. “no delirium”. The Pearson's correlation coefficient or χ2 test was used to study relationships between significant univariate variables and detect evidence of colinearity. A cutoff value of 0.85 was used as a threshold for multiple colinearity. The “coma” variable was analyzed by type of coma, and compared to patients in whom coma never occurred. Multivariate stepwise logistic regression was performed on all variables retained from univariate analysis as described above. A multivariate stepwise logistic regression was performed for each type of coma variable included as covariate. The Hosmer and Lemeshow test was used to assess the fit of the model. Two-tailed testing was conducted at a significance level of p ≤ 0.05. Analyses were performed with SAS release 8.2 (SAS Institute, Cary, N.C., USA). Mortality attributable to delirium or coma was studied using survival analysis. Survival curves were computed using the Kaplan–Meier formulas. Equivalence of survival functions between the two arms was tested using a Cox model. More precisely, a Cox proportional hazard model was adjusted with group (“delirium” vs. “no delirium”), coma (“iatrogenic coma” vs. “no iatrogenic coma”), age, and APACHE as covariates.
Results
The risk of developing delirium was significantly associated with a higher admission APACHE II score (17.9 ± 8.2 vs. 14.0 ± 8.1; p < 0.0001) but not with age (64.5 ± 14.1 vs. 62.8 ± 14.7 years), sex (147:96 vs. 303:218), or admission features, including diagnosis. A history of prior or current neurological illness did not increase the risk (p = 0.77), nor did abnormalities in bilirubin, albumin, or hemoglobin. Table 1 presents risk factors with a p value below 0.15 on univariate logistic regression. Based on multivariate analysis, patients with a history of hypertension (OR 1.88, 95% CI 1.3–2.6) and alcoholism (OR 2.03, CI 1.26–3.25) were more likely to develop delirium. Severity of illness on admission was also independently associated with the risk of delirium. On multivariate analysis each increment in APACHE II score augmented the risk of delirium by 4.9% (OR 1.049, CI 1.028–1.07, p < 0.0001). APACHE II score calculated without the GCS component [9] did not alter these results. The use of sedatives or analgesics (e. g., benzodiazepines, opiates, propofol, or epidural analgesia) did not differ in patients with vs. without delirium. The average daily dose of benzodiazepines (expressed as lorazepam equivalents) [34] was 2.7 ± 5.6 vs. 1.03 ± 4.23 mg in patients with vs. without delirium; the mean daily opioid dose were 5.3 ± 10.1 vs. 8.9 ± 24.3 mg (morphine equivalents [32]) in patients with vs. without delirium. Corticosteroid administration occurred in 216 patients (26%) and indomethacin in 53 (6%). Neither was associated with delirium.
Of the 243 patients with delirium 93 (38.3%) also had one type of coma within the first 5 days of admission. Of the 521 patients without delirium 68 (13%) had coma during the same time period (p < 0.05, χ2 test; see multivariate analysis below; Fig. 1). Thirty-three patients with iatrogenic coma had the highest risk of delirium (OR 3.22, CI 1.52–6.81), followed by those with multifactorial coma (OR 2.77, CI 1.16–6.64), and transient iatrogenic coma (OR 2.19, CI 1.3–3.7). Medical coma as covariate was not significantly associated with delirium in the multivariate model. When all coma types associated with medication use were combined in the multivariate model, the risk of developing delirium remained high (OR 3.71, CI 2.32–5.9, p < 0.0001). Of the 31 patients with prolonged coma who survived longer than > 5 days 8 (26%) developed delirium 7–44 days after ICU admission. The remaining patients died comatose.
Based on multivariate model, there was a small but statistically significant difference in pain scores (NRS) between patients with delirium (0.94 ± 1.4) and without delirium (1.43 ± 2.05; OR 0.87, CI 0.80–0.97). Sedation (RASS) scores did not differ significantly in patients with and without delirium (0.61 ± 0.8 vs. 0.23 ± 0.77, p = 0.69). Anxiety was more likely to occur in patients with than in those with without delirium (OR 1.8, CI 1.04–3.37, p = 0.03). Patients with delirium stayed in the ICU (11.5 ± 11.5 vs. 4.4 ± 3.9 days, p ≤ 0.005) and in the hospital (18.2 ± 15.7 vs. 13.2 ± 19 days, p ≤ 0.005) longer. Overall mortality was 13% in ICU and 27% in hospital. Patients with delirium were more likely to die in the ICU (20% vs. 10%, p < 0.005) and in hospital (31% vs. 24%, p < 0.005). Time to mortality in both groups is shown in Fig. 2. Delirium increased mortality in all patients (OR 1.47, CI 1.15–1.89, p = 0.0022) after adjustment for age and APACHE II score. Iatrogenic coma did not affect mortality independently (OR 1.35, CI 0.85–2.13, p = 0.2024) after adjustment for age and APACHE II score. The corresponding Kaplan–Meier curves are shown in Fig. 3.
Discussion
The 31.8% incidence of delirium in this study resembles previous reports [10, 11, 12, 13, 14] and is lower than the incidence higher than 80% suggested by others [6, 7, 8, 9]. This important discrepancy may reflect differences in patient characteristics (e. g., case mix, body weight), interpretation of what constitutes delirium, the screening instrument and its application, local sedation practices, and the confounding influence of medication-associated coma.
The Intensive Care Delirium Screening Checklist (ICDSC) [22] was used in this study because its value has been corroborated in both medical and surgical patients. The ICDSC validation included 94% of ICU admissions [22], in contrast to the 44% of 86 sequentially admitted patients in the Confusion Assessment Method–ICU (CAM-ICU)-validation [7]. Moreover, the ICDSC study included patients with neurological or psychiatric diagnoses, or abnormal consciousness on admission, and thus incorporated many patients who were excluded in substantiating the CAM-ICU [22]. The ICDSC is administered by ICU caregivers and was validated with a clinical psychiatric diagnosis [10]; abnormal scores occurring only between midnight and 8 a. m. were found in 40% of directly observed patients. Sedated patients were not considered delirious. In contrast, the CAM-ICU [7, 9] is initiated with GCS or RASS changes [33, 34]. In the “attention screening examination” patients look at a set of images which they later identify from a larger set of images. Patients are also assessed for either cognitive abnormalities or fluctuation in level of consciousness. Three of four positive items confirm the diagnosis of delirium. The required information can be obtained from chart review or from conversations with the patient's family or nurse [6, 7, 9].
The incidence of delirium may be overstated in some CAM-ICU reports [7]. Most important is the issue of what constitutes delirium. Drug-induced sedation is a desired and expected effect in the ICU. It does not, in our opinion, constitute delirium. Lin et al. [13] reported a delirium incidence of 22% using the CAM-ICU when unarousable medicated patients were excluded. Ely et al. [9] reported a delirium incidence of 80% without specifying if patients were arousable and/or under the influence of medication. Moreover the GCS, used in the initial CAM ICU screening, has only been validated in the initial assessment of neurotrauma. Finally, the direct and repeated examination of patients for clinical symptoms of delirium is likely to be more reliable than chart review [37]. Sedative use in our study was low; when unrelated to coma, it was not associated with development of delirium. The mean daily benzodiazepines doses that we report in delirious patients are lower than those noted by others [9], as are the mean daily opioid doses, which were 8.9 ± 24.3 mg morphine equivalents in our study, vs. doses of between 17–78 mg in reports describing higher delirium incidences [9]. Small doses of sedatives do not predispose to delirium. Doses sufficient to cause coma may.
Although delirium has been described as a transition between normal cognition and coma [16], this notion has not been validated in the critically ill. Coma from a primary neurological illness, such as stroke or subarachnoid hemorrhage, was not associated with delirium. This study, the first to include patients with coma or neurological illness on admission, suggests that coma is a risk factor for delirium only when sedative medications are administered, not when the cause of the coma is a primary neurological problem. Lin et al. [13] and Ely et al. [7] report that delirium in the critical care setting significantly increases ICU and total hospital length of stay, and the risk of death. Since excessive sedation and coma can both prolong length of stay, it is important to differentiate between the effect of sedation and that of coma, regardless of cause, on clinical outcome.
Delirium increased the risk of mortality after adjusting for admission APACHE scores and patient age and was more likely when coma was medication induced. Medication-related coma did not in itself confer an increased risk of death when APACHE scores, age, and delirium were considered. Confusing the diagnosis of coma with that of delirium or diagnosing delirium in the presence of coma can have two undesirable consequences. It may lead to an inflated estimate of the incidence of delirium and may also alter the mortality attributable to delirium. These factors may partially explain the differences between reports estimating the incidence of delirium at 10–30% [11, 12, 13] compared to those suggesting an incidence of over 80% [6, 7, 8, 9].
Self-reported anxiety differed between delirious and nondelirious patients, despite comparable RASS sedation scale scores. ICU patients may experience anxiety [38], and clinicians fail to detect it, despite its estimated prevalence of 25% [39]. Patients [3] and survivors [2, 40, 41] report fear accompanying hallucinations and disorientation [41]. Such patients respond to reassurance [41]. The current findings strongly suggest that anxiety should be routinely evaluated and addressed in the ICU independent of sedation. The current data confirm earlier work [10] suggesting that alcoholism and hypertension are important predictors of ICU delirium. Spies et al. [42] have elegantly emphasized the importance of alcohol use as a risk factor for neurocognitive and other ICU complications. Chronic hypertension has been associated with impairment in memory, attention, and abstract reasoning [43]. Age did not influence the occurrence of delirium in this ICU cohort, in keeping with the observations of others [9]. This contrasts with the well established risk which age confers on the likelihood of delirium in medical, surgical, and geriatric populations outside the ICU [44]. Corticosteroids [29] and indomethacin [30], previously linked to delirium in other settings, did not alter ICU delirium risk. Pain levels were minimally different between delirious and nondelirious individuals, and were lower in the delirium group. Thus the previously reported association between postoperative rest pain and delirium [31] may not occur in the ICU population, or may not be important in the setting of adequate analgesia.
All patients with “iatrogenic coma” in our cohort received continuous infusions of opiates as well as infusions or intermittent doses of sedatives (with or without titration). Protracted infusions of midazolam, but not opiates, have been associated with neurological abnormalities [45]. Transient iatrogenic coma, following direct transfer from surgery or from temporary sedation, was also associated with delirium, although to a lesser degree. This finding, and the independence of the association of APACHE and coma with delirium, makes it less likely that overall severity of illness is the determining risk factor for delirium. Patients with coma of neurological origin for more than 5 days were not analyzed because of their high mortality (80% in this study) and the inability to perform cognitive evaluation. The small patient numbers precluded statistical analysis. Among the 31 patients who survived until screening for delirium was possible, but who were not included in the risk factor analysis, delirium occurred in eight patients (26% of the group). Considering brain dysfunction in the critically ill as a single syndrome [17, 18] is thus not supported by the current study.
Conclusions
Delirium occurs in approx. 30% of critically ill patients and is associated with a history of hypertension and alcoholism, higher APACHE scores, and with clinical effects of sedative and analgesic drugs. It is unlikely that in the critically ill all structural and nonstructural CNS dysfunction conforms to a single mechanistic pathway. Prospective studies have yet to determine whether prevention, early diagnosis, or treatment of ICU delirium improve outcome.
References
Breitbart W, Gibson C, Tremblay A (2002) The delirium experience: delirium recall and delirium-related distress in hospitalized patients with cancer, their spouses/caregivers, and their nurses. Psychosomatics 43:183–194
Granberg A, Bergbom Engberg I, Lundberg D (1998) Patients' experience of being critically ill or severely injured and cared for in an intensive care unit in relation to the ICU syndrome. I. Intensive Crit Care Nurs 14:294–307
Granberg-Axell A, Bergbom I, Lundberg D (2001) Clinical signs of ICU syndrome/delirium: an observational study. Intensive Crit Care Nurs 17:72–93
Jones WHS (1931) Hippocrates (460–375 bc). Aphorisms, IV. Hippocrates. Loeb Classical Library 1
Armstrong SC, Cozza KL, Watanabe KS (1997) The misdiagnosis of delirium. Psychosomatics 38:433–439
Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, Truman B, Dittus R, Bernard R, Inouye SK (2001) The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med 27:1892–1900
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, Hart RP, Dittus R (2001) Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 286:2703–2710
Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautam S, Bernard GR, Inouye SK (2001) Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 29:1370–1379
Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE Jr, Inouye SK, Bernard GR, Dittus RS (2004) Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 291:1753–1762
Dubois MJ, Bergeron N, Dumont M, Dial S, Skrobik Y (2001) Delirium in an intensive care unit: a study of risk factors. Intensive Care Med 27:1297–1304
Aldemir M, Ozen S, Kara IH, Sir A, Bac B (2001) Predisposing factors for delirium in the surgical intensive care unit. Crit Care 5:265–270
Kishi Y, Iwasaki Y, Takezawa K, Kurosawa H, Endo S (1995) Delirium in critical care unit patients admitted through an emergency room. Gen Hosp Psychiatry 17:371–379
Lin SM, Liu CY, Wang CH, Lin HC, Huang CD, Huang PY, Fang YF, Shieh MH, Kuo HP (2004) The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med 32:2254–2259
McNicoll L, Pisani MA, Zhang Y, Ely EW, Siegel MD, Inouye SK (2003) Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc 51:591–598
Caraceni A, Grassi L (2003) Delirium—acute confusional states in palliative medicine. Oxford University Press, New York
Plum F, Posner J (1980) The Diagnosis of stupor and coma. Davis, Philadelphia
Trzepacz PT (1999) Update on the neuropathogenesis of delirium. Dement Geriatr Cogn Disord 10:330–334
Trzepacz PT (2000) Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin Clin Neuropsychiatry 5:132–148
Gardner DM, Baldessarini RJ, Waraich P (2005) Modern antipsychotic drugs: a critical overview. Can Med Assoc J 172:1703–1711
Skrobik Y (2002) Haloperidol should be used sparingly. Crit Care Med 30:2613–2614
Kress JP, Pohlman AS, O'Connor MF, Hall JB (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 342:1471–1477
Bergeron N, Dubois MJ, Dumont M, Dial S, Skrobik Y (2001) Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med 27:859–864
Amador L, Goodwin JS (2000) Postoperative delirium in the older patient. J Am Coll Surg 5:767–773
Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Falk V, Schmitt DV, Mohr FW (2004) Predictors of delirium after cardiac surgery delirium: effect of beating-heart (off-pump) surgery. J Thorac Cardiovasc Surg 127:57–64
Korevaar JC, van Munster BC, de Rooij SE (2005) Risk factors for delirium in acutely admitted elderly patients: a prospective cohort study. BMC Geriatr 5:6
Stein LM, Thienhaus OJ (1993) Hearing impairment and psychosis. Int Psychogeriatr 5:49–56
Ross D (1998) Acute neurologic complications of drug and alcohol abuse. Neurol Clin 692:503–519
Granberg Axell AI, Malmros CW, Bergbom IL, Lundberg DB (2002) Intensive care unit syndrome/delirium is associated with anemia, drug therapy and duration of ventilation treatment. Acta Anaesthesiol Scand 46:726–731
Vincent FM (1995) The neuropsychiatric complications of corticosteroid therapy. Compr Ther 21:524–528
Ananth J (1995) Musculoskeletal disorders and rheumatoid arthritis. In: Kaplan H, Sadock B (eds) Comprehensive textbook of psychiatry. Williams & Wilkins, Baltimore
Skokie I (1999) Principles of analgesic use in the treatment of acute pain and cancer pain. American Pain Society, Glenview
Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L, Marcantonio ER (1998) The impact of postoperative pain on the development of postoperative delirium. Anesth Analg 86:781–785
Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, Francis J, Speroff T, Gautam S, Margolin R, Sessler CN, Dittus RS, Bernard GR (2003) Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation–Sedation Scale (RASS). JAMA 289:2983–2991
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, Tesoro EP, Elswick RK (2002) The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 166:1338–1344
Cammarano W, Drasner K, Katz J (1998) Pain control, sedation, and use of muscle relaxants. In: Hall J, Schmidt G, Wood L (eds) Principles of critical care medicine. McGraw-Hill, New York
Lacy C, Armstrong L, Goldman M, Lance C (2004) Drug information handbook. Lexi-Comp, Hudson
Luck J, Peabody JW, Dresselhaus TR, Lee M, Glassman P (2000) How well does chart abstraction measure quality? A prospective comparison of standardized patients with the medical record. Am J Med 108:642–649
Lemos J de, Tweeddale M, Chittock D (2000) Measuring quality of sedation in adult mechanically ventilated critically ill patients. the Vancouver Interaction and Calmness Scale. Sedation Focus Group. J Clin Epidemiol 53:908–919
Rincon HG, Granados M, Unutzer J, Gomez M, Duran R, Badiel M, Salas C, Martinez J, Mejia J, Ordonez C, Florez N, Rosso F, Echeverri P (2001) Prevalence, detection and treatment of anxiety, depression, and delirium in the adult critical care unit. Psychosomatics 42:391–396
Granberg A, Engberg IB, Lundberg D (1999) Acute confusion and unreal experiences in intensive care patients in relation to the ICU syndrome. II. Intensive Crit Care Nurs 15:19–33
Hernandez G, de la Fuente R, Romero C, Naranjo ME, Zanolli M, Barticevic N, Castillo L, Bugedo G (2004) Memories and perceptions in ICU survivors: a multidimensional questionnaire. Intensive Care Med 30(Suppl A):579
Spies CD, Otter HE, Huske B, Sinha P, Neumann T, Rettig J, Lenzenhuber E, Kox WJ, Sellers EM (2003) Alcohol withdrawal severity is decreased by symptom-orientated adjusted bolus therapy in the ICU. Intensive Care Med 29:2230–2238
Waldstein SR, Manuck SB, Ryan CM, Muldoon MF (1991) Neuropsychological correlates of hypertension: review and methodologic considerations. Psychol Bull 110:451–468
Inouye SK, Bogardus ST Jr, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, Cooney LM Jr (1999) A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 340:669–676
McKenzie CA, McKinnon W, Naughton DP, Treacher D, Davies G, Phillips GJ, Hilton PJ (2004) Differentiating midazolam over-sedation from neurological damage in the intensive care unit. Crit Care 9:32–36
Acknowledgements
The authors sincerely thank Drs. Daren Heyland and John Marshall for their critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-0400-6
Appendix: Intensive Care Delirium Screening Checklist
Appendix: Intensive Care Delirium Screening Checklist
Examination are carried out on days 1–5 using a scale based on information collected from each entire 8-h shift or from the previous 24 h. Patients are assigned values on the following items of 1 (obvious manifestation of the item) or 0 (no manifestation of an item or no assessment possible); the total score ranges from 0 to 8.
-
1.
Altered level of consciousness. No response (A) or the need for vigorous stimulation in order to obtain any response (B) signifies a severe alteration in the level of consciousness and precludes evaluation. If there is coma (A) or stupor (B) no score is entered, and there is no further evaluation during that period.
-
A: No response (no score).
-
B: Response to intense and repeated stimulation (loud voice and pain; no score).
-
C: Response to mild or moderate stimulation; drowsiness or requirement of a mild to moderate stimulation for a response implies an altered level of consciousness (1 point).
-
D: Normal wakefulness; wakefulness or sleeping state that can easily be aroused (0 point).
-
E: Exaggerated response to normal stimulation; hypervigilance is rated as an abnormal level of consciousness (1 point).
-
-
2.
Inattention; difficulty in following a conversation or instructions, easily distracted by external stimuli, difficulty in shifting focuses (1 point).
-
3.
Disorientation; any obvious mistake in time, place, or person (1 point).
-
4.
Hallucination, delusion, psychosis; the unequivocal clinical manifestation of hallucination or of behavior probably due to hallucination (e. g., trying to catch a nonexistent object) or delusion; gross impairment in reality testing (1 point).
-
5.
Psychomotor agitation or retardation; hyperactivity requiring the use of additional sedative drugs or restraints in order to control potential danger to oneself or others (e. g., pulling out intravenous lines, hitting staff); hypoactivity or clinically noticeable psychomotor slowing (1 point).
-
6.
Inappropriate speech or mood; inappropriate, disorganized or incoherent speech; inappropriate display of emotion related to events or situation (1 point).
-
7.
Sleep/wake cycle disturbance; sleeping less than 4 h or waking frequently at night (do not consider wakefulness initiated by medical staff or loud environment); sleeping during most of the day (1 point).
-
8.
Symptom fluctuation; fluctuation of the manifestation of any item or symptom over 24 h (e. g., from one shift to another; 1 point).
Rights and permissions
About this article
Cite this article
Ouimet, S., Kavanagh, B.P., Gottfried, S.B. et al. Incidence, risk factors and consequences of ICU delirium. Intensive Care Med 33, 66–73 (2007). https://doi.org/10.1007/s00134-006-0399-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0399-8